AML Treatment In The Works? Rare Form Of Leukemia Found To Originate In Pre-Leukemic Stem Cells
An aggressive form of blood cancer may see improved treatment following Canadian researchers’ study of stem cells, specifically those that mimic normal blood cells and eventually lead to relapse.
Contrary to much of the cancer research surrounding acute myeloid leukemia (AML), relapse after remission doesn’t necessarily indicate a failure of chemotherapy, according to lead researcher and stem cell scientist, Dr. John Dick. His team’s new findings provide evidence that the real culprit could be pre-leukemic stem cells found in the patient’s bone marrow. The discovery could one day lead to the development of drugs that specifically target the gene causing many of the cells’ malfunctions.
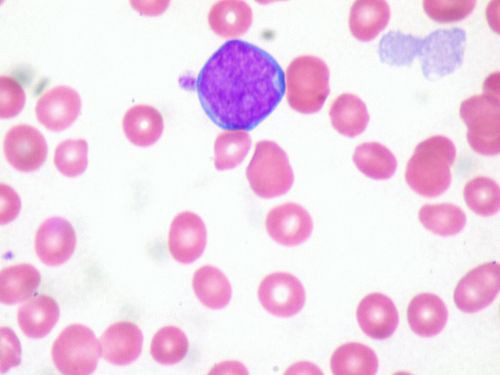
Leukemia is a cancer of the blood or bone marrow, where immature white blood cells multiply rapidly. AML is unique in that it refers specifically to the blood-forming tissue of the bone marrow, where the white blood cells proliferate abnormally. It accounts for roughly 1.2 percent of cancer cases. But in recent years, Dick explains, scientists have learned about pre-leukemic stem cells that reside in clusters in the same location.
"Now we have a potential tool for earlier diagnosis that may allow early intervention before the development of full AML,” Dick, who discovered leukemia stem cells in 1994 and colon cancer stem cells in 2007, said in a statement. “We can also monitor remission and initiate therapy to target the pre-leukemic stem cell to prevent relapse.”
Dick and his team found that 25 percent of AML patients carried a mutation on the DNMT3a gene. This mutation causes harmful pre-leukemic cells to function like the body’s normal supply of blood cells, growing abnormally and capable of surviving chemotherapy. After the treatment, the cells, which have since made a home in the patient’s marrow, now resurface to form a reservoir of cells that may eventually mutate again, leading to relapse.
"Our discovery lays the groundwork to detect and target the pre-leukemic stem cell and thereby potentially stop the disease at a very early stage when it may be more amenable to treatment,” Dick explained.
After more than six years of experiments in the lab involving mice genetically engineered to accept human forms of AML without rejection, and together with the genomic analysis of more than 100 leukemia genes, Dick and a team of oncologists were able to pinpoint pre-leukemic stem cells’ location. Now, the team claims its understanding of how this type of cancer forms opens the doors for targeted pharmacological approaches.
"By peering into the black box of how cancer develops during the months and years prior to when it is first diagnosed, we have demonstrated a unique finding,” Dick said. “Our study suggests that in some cases the chemotherapy does, in fact, eradicate AML; what it does not touch are the pre-leukemic stem cells that can trigger another round of AML development and ultimately disease relapse.”
In the future, the findings should allow doctors to check AML patients for other forms of non-blood cancer based on their observed mutations.
Source: Shlush L, Zandi S, Mitchell A. Identification of pre-leukaemic haematopoietic stem cells in acute leukaemia. Nature. 2014.



























