Anti-Depressants: The Newest Weapon Against Deadly Lung Cancer?
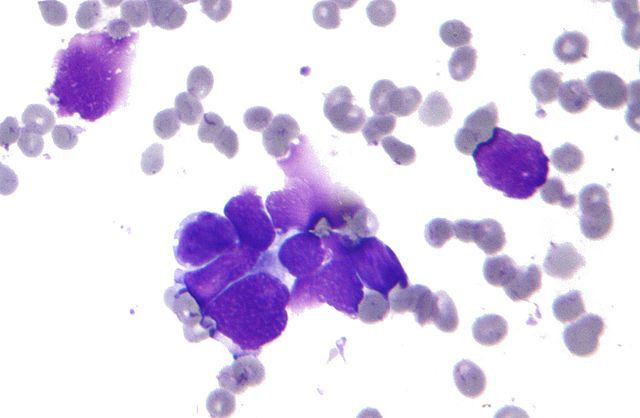
Revisiting old research, Stanford scientists discovered two anti-depressants that effectively treated small-cell lung cancer (SCLC) in animal models. Specifically, the two Food and Drug Administration (FDA)-approved drugs, imipramine and promethazine, activated a cellular self-destruct pathway that killed the cancer cells. Currently, there are no approved targeted therapies for small-cell lung cancers, which are of neuroendocrine origin and known to be particularly deadly.
"The five-year survival for small-cell lung cancer is only five percent," Julien Sage, senior author and associate professor of pediatrics and genetics at Stanford University School of Medicine, stated in a press release. "There has not been a single efficient therapy developed in the last 30 years. But when we began to test these drugs in human cancer cells grown in a dish and in a mouse model, they worked, and they worked, and they worked."
Experimental Design
To conduct their study of potential treatments for SCLC, the researchers used bioinformatics, a process by which computer technology is applied to databases of biological and biochemical information. Atul Butte, co-author and director of the Center for Pediatric Bioinformatics at Lucile Packard Children's Hospital at Stanford, had previously developed his own computerized 'discovery pipeline' with former faculty member Joel Dudley, another co-author of the current study. Through this method of investigation, researchers can spot patterns and trends undetectable until massive amounts of data are viewed all at once.
For this particular study, the researchers scanned through thousands of gene expression profiles, which had been collected from individual studies conducted by multiple researchers and stored together in large databases. The range of profiles included both normal and diseased cell types and tissues, some that had been treated with medications and others not. The researchers were looking for new potentials from old drugs.
During testing and trials, for example, a particular drug would block or suppress a particular molecular pathway routinely activated in a cancer cell, and so it only follows that the drug should be tested for the potential to treat that type of cancer — no matter what disease it had been originally developed to treat. And after identifying a potential new use for an old drug, the next step would be to test it in animal models.
"This is a good example of how we can combine 'big data' and the mature field of preclinical animal models to rapidly find new uses for old drugs,” Sage stated in a press release.
Time and Money Saved
Once their bioinformatics query identified imipramine and promethazine as able to target the neuroactive ligand receptor interaction pathway and the calcium signaling pathway, the researchers generated mutant mice bearing cisplatin-resistant SCLC tumors. Conducting laboratory experiments, they found both drugs induced cell death mechanisms within the SCLC cancer cells, while imipramine inhibited the growth of chemotherapy-resistant tumors. Such evidence suggests the possibility that imipramine might also be effective against SCLCs in patients who developed resistance to standard chemotherapy. Imipramine was also found to be effective in an animal model of pancreatic neuroendocrine tumors.
Based on these results — as well as the fact that these drugs have already been FDA-approved — the researchers have already initiated a clinical trial to test their theory in patients. In fact, they are recruiting participants with small-cell lung cancer and other high-grade neuroendocrine tumors to test desipramine, another FDA-approved drug that is similar to imipramine.
"We are cutting down the decade or more and the $1 billion it can typically take to translate a laboratory finding into a successful drug treatment to about one to two years and spending about $100,000," Butte stated in a press release. He believes this "repositioning" of an existing drug serves as an example of how massive genetic and biological databases can change the face of medicine.
"From the day we started this project, it took less than 20 months to initiate a clinical trial," Sage stated in a press release.
Source: Sage J, Jachan NS, Dudley JT, et al. A Drug Repositioning Approach Identifies Tricyclic Antidepressants as Inhibitors of Small Cell Lung Cancer and Other Neuroendocrine Tumors. Cancer Discovery. 2013.



























