Birth Control May Be Dropped As Family Doctor Training Requirement
Every seven years: the Book of Deuteronomy commands a release of the poor from debt, lovers squelch the "Seven Year Itch," and the human body completes a regenerative cellular cycle.
The sabbatical year is also the time for the Accreditation Council for Graduate Medical Education to rewrite curriculum for each medical specialty, including the training young clinicians receive in reproductive health.
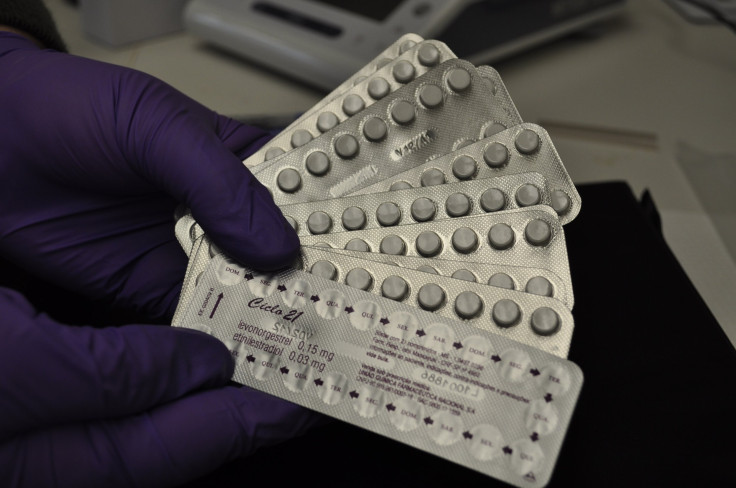
The group will accept public commentary until Thursday on a proposal to eliminate requirements to train family physicians in methods of contraception, even as new federal law makes such contraceptives more available to women.
Dr. Linda Prine, a family physician from New York, says the rule change for graduate medical education in the specialty would greatly affect women receiving care outside of major cities, where most see family doctors as opposed to obstetrician-gynecologists.
For the majority of women, particularly outside major cities, it's family doctors, not obstetrician-gynecologists, who provide for their reproductive health needs. "The main people who staff community health centers, as well as large swaths of rural America, are family doctors," she said. To become a family physician, formerly known as a general practitioner, medical residents must complete an intensive three-year program approved by the group.
Dr. Prine, who is also the medical director of the Reproductive Health Access Project, helped to institute birth control as part of the curriculum seven years ago. The change requires all residents in that specialty to learn about contraceptives beyond the birth control pill, including intrauterine devices and implants — and to counsel patients with unwanted pregnancies on options including abortion.
"The language was put in so that we would be assured that family doctors were prepared to provide health care for their patients," she said.
That graduate medical curriculum, however, did not meet with universal approval, said Peter Carek, a professor of family medicine at the Medical University of South Carolina and chairman of the curriculum-writing committee for family medical residents. "The feedback we've gotten over the years is that a lot of the curricular requirements were too specific," he said. "So in general what we've tried to do as a committee is to at least in as many areas as we could, pull back some of those specific requirements and give them more general requirements to follow," he said.
Dr. Prine told NPR Friday she thinks leaving the contraceptive training to individual programs would hurt reproductive medicine, given that many hospital systems are run by religious groups that oppose contraception.
"The way it works right now, the residency is required to at least send the residents off-site to another place, say, a family planning clinic where they can learn how to provide birth control," Dr. Prine said. "If these regulations change and there's no wording whatsoever about the need to provide contraception, the residency programs would no longer be obliged to send their residents somewhere where they would get this education."
Thirteen of the 25 largest health systems in the U.S. are run by religious institutions, including 11 run by the Catholic Church - which is suing the federal government over a new requirement they provide birth as part of employee health insurance coverage.
Also, see Catholic Church Drops White House Subpoena Request, Continues Contraceptives Fight and listen to NPR's coverage.
Published by Medicaldaily.com



























