Blood Test Screens For Diabetes In At-Risk Population: Could Diagnosis Really Be This Simple?
Despite its longstanding role as one of the most effective ways to track a diabetic’s health, the A1c blood test has never been widely used to predict the disease’s onset. Now, through one of the most comprehensive studies of its kind, researchers from Tel Aviv University have shown the blood glucose test can successfully predict a person’s risk for diabetes and quantify this risk as the levels increase.
When it comes to the way we perform health care, the U.S. is notoriously a treatment country. Preventive medicines get far less attention than the cocktail of anti-inflammatories, antidepressants, anticoagulants, and anti-anxiety drugs currently offered to patients. As more than one-third of all U.S. adults are overweight, according to the Centers for Disease Control and Prevention (CDC), preventing the complications that go with obesity becomes more urgent. Diabetes falls into this category.
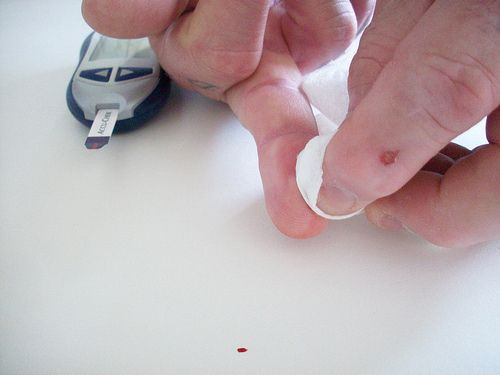
The CDC estimates that approximately 25.8 million Americans have type 2 diabetes. Worse, 79 million have prediabetes, a condition characterized by dangerously high blood sugar levels that, if left untreated, could easily tip into full-blown diabetes. The American Diabetes Association recommends patients regularly check their blood glucose levels to ensure this tip doesn’t happen, particularly if the person is taking insulin or cannot manage his or her glucose independently. A healthy level, as judged by the A1c test, falls below 5.7 percent.
Accordingly, researchers found that since patients received the predictive A1c test between 2002 and 2005, at-risk subjects were significantly more likely to develop diabetes if their levels were as low as 5.5 percent than subjects whose levels were below 5.5 percent. And each additional 0.5 percent increase doubled a person’s risk for the disease, up to 7 percent. Being obese also doubled a person’s risk for diabetes.
A total of 10,201 patients comprised the team’s study. Over the four years, 22.5 percent developed type 2 diabetes, the most common form of the disease, within five to eight years. This signaled to researchers that A1c may deserve a home in the toolkit of doctors looking to prevent diabetes in at-risk patients.
"Our study supports the idea that the A1c test, used to diagnose type-2 diabetes, can also be used at a much earlier stage to screen for the disease in the high risk population, like overweight patients," said Dr. Nataly Lerner, study leader, in a statement.
Type 2 diabetes is characterized by a surplus of glucose in the body, which arises due to the inability to produce enough insulin. A hormone produced in the pancreas, insulin helps regulate blood glucose levels. For diabetics who can’t regulate the glucose through their diet, they must receive daily insulin injections to balance the levels out.
Researchers argue that A1c is but another measure in the physician’s arsenal, along with measures of family history, a patient’s diet, exercise level, and obesity, which can be used to stop diabetes in its tracks. "We were actually able to quantify how risk increases with A1c levels," Lerner concluded. "This could allow doctors to make more informed decisions regarding diabetes prevention."
Source: Lerner N, Shani M, Vinker S. Predicting type 2 diabetes mellitus using haemoglobin A1c: A community-based historic cohort study. European Journal of General Practice. 2013.



























