Botched Surgery: Doctors' 'Never Events' Tied To Mental Fatigue, Breaking The Rules
In the past month, doctors from around the world have been posting photos of themselves sleeping while on the job to social media. The movement, born from a supportive response to a single photo of a resident in Mexico who was caught sleeping, sought to highlight the grueling schedules and amount of work a doctor has to put up with on a daily basis (shifts can often last as long as 36 hours). That said, it’s not surprising their mental stamina might waver, making them more prone to mistakes — some of which, unfortunately, end up occurring on the operating table.
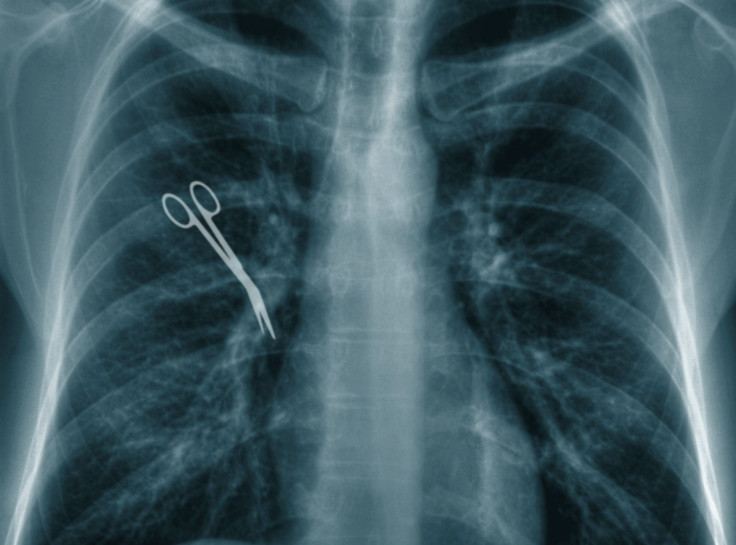
We often call these mistakes botched surgeries, though they’re better known in the medical community as surgical “never events.” They occur in about one of every 12,000 patients, and often involve a foreign object being left in the body, an operation being completed on the wrong side or area of the body, a wrong implant, or the wrong procedure altogether. Why do they happen? As mentioned above, a new study suggests doctors’ excessive workloads may be taking a toll on their mental stamina, and thus their ability to make decisions and communicate effectively.
Researchers from Mayo Clinic came to this conclusion after looking into the clinic’s own never events. They used a system created to investigate military plane crashes, called Human Factors Analysis and Classification System, to look at factors that might have contributed to the mistakes, including environmental, organizational, job, and individual characteristics. They looked at 69 never events among 1.5 million invasive procedures performed over five years. Broken down, 24 operations involved the wrong procedure, 22 occurred in the wrong area or side of the body, five involved the wrong implant, and in 18 operations, objects were left inside the body.
For each event, the Mayo researchers found there were about four to nine factors that contributed to the mistake, amounting to 628 total factors. All of them fit into one of four categories: “Preconditions for action,” including poor hand-offs, distractions, overconfidence, stress, mental fatigue, and ineffective communication — focusing too much on a single task while forgetting about the bigger picture also fit in here. The other categories included unsafe actions, such as bending or breaking rules or failing to understand the procedure; oversight and supervisory factors, such as inadequate supervision and planning problems; and organizational problems.
“What it tells you is that multiple things have to happen for an error to happen,” said Dr. Juliane Bingener, a gastroenterologic surgeon at Mayo Clinic. “We need to make sure that the team is vigilant and knows that it is not only OK but is critical that team members alert each other to potential problems. Speaking up and taking advantage of all the team’s capacity to prevent errors is very important, and adding systems approaches as well.”
Hospitals already have numerous systems in place to prevent most never events. For example, computer systems at some hospitals now track sponges, one of the most common items left in the body, through a barcode scanning system. Other measures already in place include team briefings before surgery starts, a pause before the first incision is made, and debriefings after surgery that include a World Health Organization-recommended checklist.
Still, in hopes of reducing rates of never events even more, the researchers recommended special attention be paid to the doctors who make up the team, the technology they’re using, their schedules, and the possibility they’re fatigued.
Source: Thiels C, Mohan T, Nienow J, et al. Surgical never events and contributing human factors. Surgery. 2015.
Published by Medicaldaily.com



























