Cancer Detection With MRI As Effective As PET-CT Scan, But With Zero Radiation Risks
As a way to avoid heavy radiation exposure during cancer detection, scientists from Stanford University’s School of Medicine and Lucile Packard Children’s Hospital have demonstrated that MRI-based imaging techniques are just as effective as conventional scanning methods, but bring none of the risks.
Finding cancerous tumors before they spread is a critical part of the disease’s prevention. Unfortunately, one of the most effective ways to find them is to send radioactive tracers swimming through the body, as part of PET-CT scan, exposing patients to the equivalent of 700 chest X-rays. Among children especially, whose bodies and brains are still developing, high-level exposure to radiation could lead to secondary forms of cancer later in life. This risk-reward dilemma prompted the team to investigate the safety and effectiveness of MRI-based approaches, which mimic a PET-CT scan’s results, but bear none of the costs.
"I'm excited about having an imaging test for cancer patients that requires zero radiation exposure," said senior author of the study, Dr. Heike Daldrup-Link, associate professor of radiology at Stanford and a diagnostic radiologist at the hospital, in a statement. "That is a big deal."
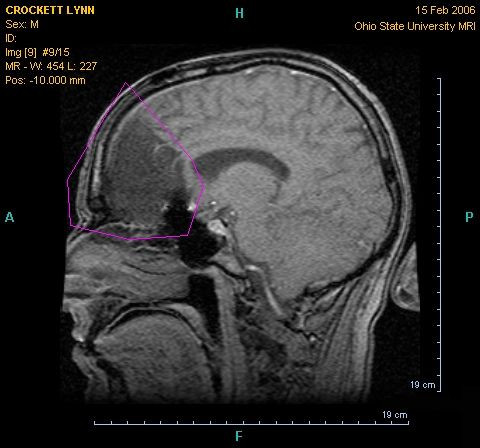
Traditional PET-CT (positron emission tomography-computed tomography) scans utilize the dual power of the PET scan, which locates a radioactive isotope injected into a patient’s desired tissues, and a CT scan, which produces a 3-D model of the body via X-rays. In the team’s current study, involving 22 patients ages 8 to 33 who had lymphoma or sarcoma, PET-CT scans found 163 of 174 total tumors.
Meanwhile, some research suggests that one PET-CT scan exposes a person to the same amount of radiation that employees who work with radiation directly can safely be exposed to in a year. And while the risk of cancer arises at levels five times that amount, experts fear that early exposure in life increases a child’s risk for cancer, particularly as they have many years left to develop it. Daldrup-Link and her colleagues sought to solve this problem with MRI-based techniques.
"Some type of whole-body MRI imaging test is available at many big children's hospitals right now," Daldrup-Link said, adding that hesitant doctors have remained withdrawn because of a lack of confidence. "It's slowly entering clinical practice, but clinicians are cautious and want to be convinced.”
The team hopes their current study changes that, as the MRI scans found 158 of 174 total tumors. As opposed to an injectable tracer that courses through the patient’s body, these scans work via a contrasting agent made up of iron nanoparticles. The nanoparticles stay in the body for many days, and when scanned, reveal blood vessels as brighter and important organs and components, such as livers, spleens, and bone marrow, as darker — providing a contrast to see tumors in greater relief. The U.S. Food and Drug Administration has approved the nanoparticles to treat anemia, and the team received permission for experimental use.
Overall, the two methods produced similar levels of sensitivity, specificity, and diagnostic accuracy. Despite a small risk of allergic reaction to the nanoparticles' coating, the MRI scans yielded no negative side-effects among subjects. With their latest success, the team has plans for future research to encompass all aspects of cancer treatment, from early stages to later stages that includes a broader pool of patients with more diverse forms of the disease.
"It's really exciting that this will soon be clinically applicable," Daldrup-Link said.
Source: Klenk C, Gawande R, Uslu L, et al. Ionising radiation-free whole-body MRI versus ¹⁸F-fluorodeoxyglucose PET/CT scans for children and young adults with cancer: a prospective, non-randomised, single-centre study. The Lancet. 2014.
Published by Medicaldaily.com



























