CDC Estimates New Antibiotic Resistance Initiative Will Save 37,000 Lives Over 5 Years

A coordinated national effort might prevent 619,000 patients from becoming infected with antibiotic-resistant germs and save a total of 37,000 lives over five years, estimates the Centers for Disease Control and Prevention (CDC). Up to 70 percent of infections caused by so-called “nightmare germs” known as CRE (carbapenem-resistant Enterobacteriaceae) also might be prevented over that same period, CDC projected in a new model released on Tuesday in support of its $264 million antibiotic resistance solutions initiative.
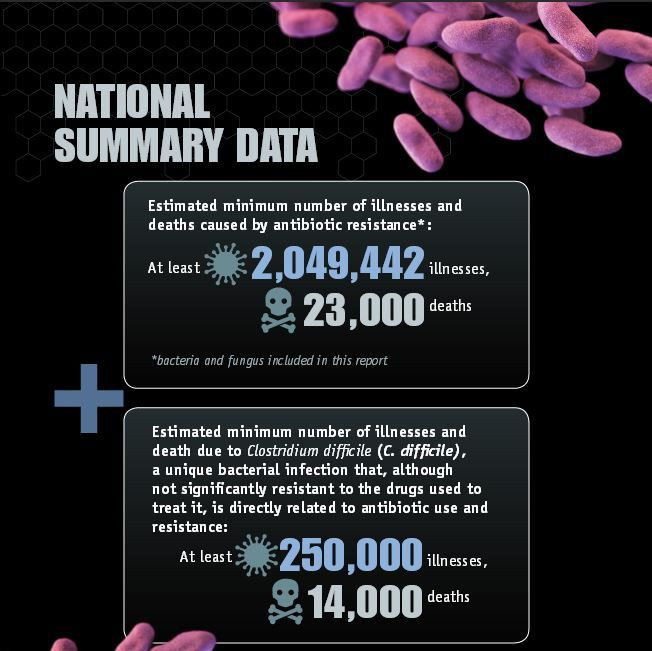
While antibiotic drugs save millions of lives each year, antibiotic-resistant bacterial strains cause at least two million illnesses and 23,000 deaths annually in the United States alone. Antibiotic resistance refers to when bacteria or "bugs" continue to thrive inside patients' bodies, making them sick even after they've taken medicine to kill the germs. Because of their ability to survive most drugs, such resistant bacteria are referred to as "superbugs."
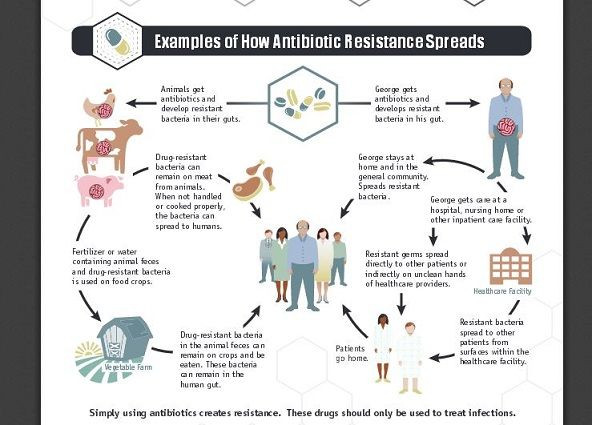
CRE germs, in particular, have become resistant to all or nearly all antibiotics currently available. Commonly, CRE infections spread between health care facilities, including hospitals and nursing homes, harming the most vulnerable.
Among the other most urgent threats are Clostridium difficile (C. difficile or C. diff) bacteria, which are passed in feces and spread to food, surfaces, or objects. These bacteria are naturally resistant to many drugs and cause an estimated 14,000 deaths each year. As Mayo Clinic explains, studies show increasing rates of C. diff infections among people usually considered low risk, such as younger and healthy individuals without a history of antibiotic use or exposure to hospitals and nursing homes.
MRSA (methicillin-resistant Staphylococcus aureus) can cause pneumonia and sepsis, the Mayo Clinic notes on its website. Health care-associated MRSA infections typically accompany invasive procedures or devices, such as surgeries, intravenous tubing, or artificial joints. Community-associated MRSA often begins as a painful skin boil and then, commonly, is spread by skin-to-skin contact among groups, such as high school wrestlers, child care workers, and people living in crowded conditions.
Finally, the germ Pseudomonas aeruginosa is resistant to almost all antibiotics and is the source of bloodstream infections in hospital patients when it spreads either on the hands of health care workers or by contaminated equipment that is improperly cleaned. This germ, too, is now appearing in the wider community and harming healthy young people, according to the CDC.
CDC has modeled how a coordinated effort might reduce the number of CRE infections after this deadly bacteria enters 10 facilities in an area sharing patients. If independent action on the part of a single facility would result in 1,500 patients getting CRE, a coordinated approach — where all the facilities in the area work together to prevent infections and notify each other before transferring patients — the CDC predicts only 400 patients would develop an infection with CRE.
“We can dramatically reduce these infections if health care facilities, nursing homes, and public health departments work together to improve antibiotic use and infection control so patients are protected,” Dr. Tom Frieden, CDC director, stated in a press release.



























