To Choose the Right Birth Control, Know Yourself

With a new gel and a new patch joining the existing line-up of contraceptive options, it seems that women have many choices these days to prevent a pregnancy.
On the face of it, yes. Condoms, spermicide, IUDs, the pill, a cervical cap, a diaphragm, the gel, are part of the list. But the birth control a woman chooses, said experts, needs to fit her life. And her personality. A woman who has post-it notes all over her computer screen might not be the best candidate for daily medication.
Bottom line: If you want your birth control to be effective, then make sure your choice is realistic and feasible.
“The vast majority of women will be able to find a contraception that works,” said
Bethany Golden, a certified nurse midwife and PhD candidate at the University of California San Francisco, “but we still have women that can't … if someone can’t have a hormonal contraception, we’re down to a few options.”
The pill, the patch and the shot, oh my!
Finding the contraception that works for you can be complicated. So, how can you make it uncomplicated?
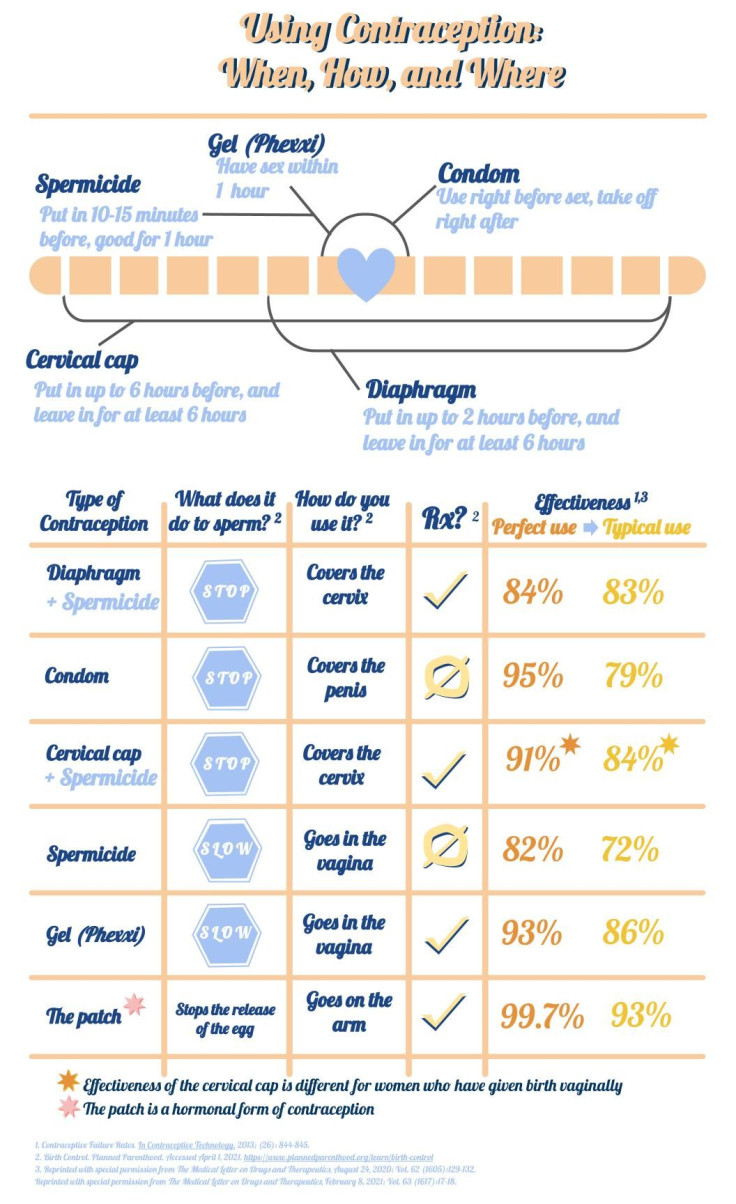
First, evaluate the product. How does it work, how is it used, and how effective is it, from two vantage points: its effectiveness for the typical user, and when it’s used exactly as the manufacturer says. Typical use includes some user error, say, genital contact before putting on a condom, or forgetting to take the pill one weekend. But the perfect use figure represents how good the method is.
Knowing the differences between these two figures and knowing what that typical error is that can result in a pregnancy can help you choose the best prophylactic. Said the author of one study: “The user characteristic that is probably most important is imperfect use of the method.”
The accompanying chart can help you decide.
Good contraception needs to be something you’ll use, and that can mean different things to different people. It might mean it fits your price point, or it is discrete. Maybe you like getting a period, maybe you hate it.
Golden explained people can change and adapt. “We all have the ability to integrate different forms of birth control, if we desire to. So the question is, is the desire there, is the motivation there, and is there a tip and trick that somebody can do.” Getting the right fit with contraception means balancing a bunch of needs and wants, and personality will come into it. “People's personalities play a factor but again, It may not be the factor that's the most critical for choice,” said Golden.
Type A
Does this sound like you ? As a condom user, you always have a condom on hand, check its expiration, and always put it on the right way?
If you said ‘yes’, that’s a perfect user.
Or the pill? Do you have a timer set to take the pill and always have the next pack ready? Or do you keep the pills near your toothbrush?
Perfect user.
But, what if that isn’t you? What if you’re the woman with post-it notes all over her computer?
Forgetful or spontaneous
For the person who can rarely find her keys and prefers intuition to a GPS, then methods like IUDs, the ring or intrauterine devices and shots have little user error. The user has little control over these types because a health care professional takes care of either placement or the shot, and so the perfect and typical use is similar. The shot and most IUDs are hormonal although the Paragard IUD, a non-hormonal contraceptive, is made of copper.
The shot lasts about 3 months and the copper IUD, about 10 years.
Frequency
Frequency is another point to consider in determining the type of contraception. Maybe you have sex infrequently but like being protected all the time by something like an IUD or an implant. Or you are more sexually active and like having long-term protection but also use condoms with different partners.
This is not one size fits all. “You could have two people with totally different frequencies, who choose the same method,” said Golden.
Other options: The ring is a hormonal birth control that sits in the vagina below the cervix. There are also the diaphragm and the cervical cap, dubbed barrier contraception, and are used with spermicide.
Narrowing the choice
The next decision is hormonal or non-hormonal. The pill, the patch, the shot, the ring and IUDs are predominantly hormonal. Condoms, spermicide, the gel, the sponge and the diaphragm are all non-hormonal.
All methods of contraception have advantages and disadvantages. And, unless a physician is involved in the birth control method -- IUD insertion, for example -- ineffective, inconsistent use is an important reason why contraception isn’t as effective as it can be.
Some hormonal birth control, like pills, can cause mood changes, spotting, nausea and breast pain although these may get better over time. In rare cases, women have developed blood clots, although this was a bigger issue in the past, when the pill had a higher dose of estrogen.
“There are effects that birth control methods have on women's bodies,” said Golden, “However, they differ from person to person.”
Patches are other types of hormonal contraception. Xulane, approved in 2014 and Twirla, approved in February 2020, each have the same shortcoming: the heavier the woman is, the less effective the patch is.
For people who don’t want to use hormonal contraception, a gel offers a DIY option, not unlike spermicide.
Phexxi, approved last spring by the FDA, is an acidic gel inserted before sex and is good for an hour. Although the idea of spreading an acidic gel inside your vagina may not seem appealing, its efficacy is backed by science. The vagina is normally a little bit acidic, and sperm is a little bit basic. By keeping the vagina acidic, the gel slows down sperm and prevents pregnancy.
The gel requires a prescription. For a comparison with unprotected sex, sperm can reach their target within minutes after ejaculation and can hang around for days.
In a clinical trial, 101 pregnancies occurred in 1,183 women over a seven-month period, bringing the cumulative pregnancy rate to 13.7%. The trial organizers did not include any menstrual cycles in which the women used an additional contraceptive. The pearl rate, a measure of how many pregnancies occur among 100 women, was 27.5.
This gel also has some side effects, including mostly minor burning. But, this side effect can be a shared experience: 9.8% of male partners reported some, mostly mild discomfort. Trial participants reported that the side effects decreased with use.
As for the patches, their efficacy is based on the woman’s weight. Xulane is only effective in women who weigh less than 198 pounds. Likewise, Plan B and Ella, both emergency contraceptives, have weight limits above which they are less effective. Plan B’s is 165 pounds and Ella’s is 195 pounds.
Discussing other differences
What is the difference between spermicide and a gel? Good question. While the gel slows sperm down, spermicide damages it. Spermicide also can increase the risk of vaginal irritation and cause itching and burning. Vaginal irritation, in turn, can leave women more vulnerable to STIs and HIV. Spermicide is a detergent, and just like hands can get dry and chapped from frequently washing or washing lots of dishes, repeated applications of spermicide into the vagina can damage the skin there.
Condoms, male and female, and spermicide come from the drug store, even the grocery store. That can be a factor in what method you have the best access to. Another point for condoms: They are the only method of contraception that can protect against STIs.
There is no 100% effective birth control. The only way not to get pregnant is to keep ejaculate out of the vagina.
Just remember if you decide to go without protection: Penetrative intercourse with no contraception, out of 100 women, could result in 85 pregnancies.
Intimate choice
Doctors and providers at many low-cost and safety net clinics can help talk you through the options and answer questions. Golden said that if a provider isn’t talking about a type of contraception you’re interested in, bring it up. Ask how frequently they prescribe it. Not all providers are as familiar or as comfortable with certain types of contraception. The trick is finding the one that works best for you.
References for the graphic
- Contraceptive Failure Rates. In Contraceptive Technology. 2013; (26): 844-845.
- Birth Control. Planned Parenthood. Accessed April 1, 2021. https://www.plannedparenthood.org/learn/birth-control
- Reprinted with special permission from The Medical Letter on Drugs and Therapeutics , August 24, 2020; Vol. 62 (1605):129-132. Reprinted with special permission from The Medical Letter on Drugs and Therapeutics , February 8, 2021; Vol. 63 (1617):17-18.



























