Cold Caps Could Prevent Hair Loss In Chemo Patients: How Safe Is A 41-Degree Head Cover?
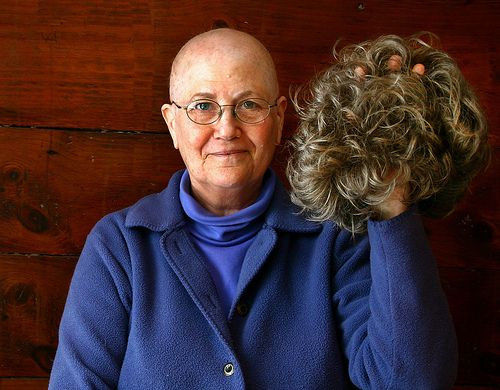
Recent tests on cold caps for chemotherapy patients showed promising results in preventing the treatment's characteristic hair loss, which, as some doctors note, can be more difficult for patients to overcome than the therapy itself.
Testing The Cold Caps
The near-freezing cold caps are chilled to 41 degrees before being tightly secured on the patient's scalp. As the cap reduces blood flow to the brain, the cancer-fighting drugs have an increasingly harder time reaching the hair follicles. This type of treatment has the potential to minimize, and ideally, erase, the stigma generated by chemo's most despised side effect, thereby encouraging patients to undergo the treatment where they otherwise would shy away.
"I didn't necessarily want to walk around the grocery store answering questions about my cancer," recalled Miriam Lipton, 45, of San Francisco. Lipton, who suffered from breast cancer, took part in a 2011 pilot-study for the cold caps and reported keeping most of her hair. "If you look OK on the outside, it can help you feel, 'OK, this is manageable, I can get through this.'"
Lipton's efforts in the study two years ago have helped spawn a larger clinical trial later this summer to test out the scalp-cooling cap, DigniCap, on 110 early stage breast cancer patients. The study is being performed by Dr. Hope Rugo of the University of California, San Francisco, and Dr. Susan Melin of North Carolina's Wake Forest Baptist Medical Center.
Safety And Effectiveness
DigniCap and other brands have existed in the scalp cooling market for decades; however, their recent prominence has emerged from studies like the one Lipton participated in, which hope to allay fears that the cold actually prevents the chemotherapy from targeting cancer cells in the scalp.
"Do they work and are they safe? Those are the two big holes. We just don't know," said American Cancer Society spokeswoman Kimberly Stump-Sutliff, an oncology nurse who said foreign studies have yet to answer that question. "We need to know."
The process of scalp cooling involves the cap being cooled to around 41 degrees and placed snugly on the user's head. Every 20 to 30 minutes the cap must be switched for a colder one.
In Lipton's study, the cooling helped her retain the majority of her bangs and hair beneath the crown. But due to the cap fitting more loosely on the top of her head, hair loss was more pronounced in that area. Her greatest side effect was the occasional headache from the cold.
"It wasn't perfect, but it was easier," said Lipton, who's healthy today. "I felt normal much more quickly."
Lipton's bout with breast cancer and subsequent test of the DigniCap comes as her second round with the illness. During the first go-around, the chemo caused all her hair to fall out — one of the most common markers of someone with cancer. It's a marker many experts say people try to avoid as much as they can, sometimes by even forgoing the therapy altogether.
"Quite frankly, it's the first or second question out of most patients' mouths when I tell them I recommend chemotherapy," said Melin. "It's not, 'Is this going to cure me? It's, 'Am I going to lose my hair?'"
The Future Of Scalp Cooling
Pending the success of Rugo and Melin's study, Sweden's Dignitana AB plans to seek U.S. Food and Drug Administration (FDA) approval to market the medical device in the U.S., the Associated Press reports. FDA approval could forge the way for diversified technology and wider use.
Despite the lack of approval, certain brands have already entered the market. Penguin Cold Caps, which are manufactured by a British company, are sold to consumers for $455 a month. Roughly 50 hospitals offer the caps to patients, who bring the caps to their chemo sessions and often bring a friend to help change the caps once they lose their chill. The caps are kept on dry ice while in transit.
The specifics of scalp cooling — i.e. who it benefits most, the optimum chilling temperature, if it works across all intensities of chemo — haven't been ironed out yet. The future for hair-preserving approaches to chemotherapy remain an issue in the forefront, however, notes Dr. Laura Esserman, a UCSF breast cancer specialist.
"If it matters to our patients, it should matter to us," she said. "It's really not more complicated than that."
Published by Medicaldaily.com



























