2 Studies, 2 Results: What to Believe About Remdesivir?
One day, a study published in the New England Journal of Medicine is picked up by the news media, who tell us that remdesivir works in the fight against COVID-19. A few days later, other stories, these based on World Health Organization research, say it doesn’t. So which result holds the truth? Neither? Both?
It's a trick question. The studies are looking at two different outcomes.
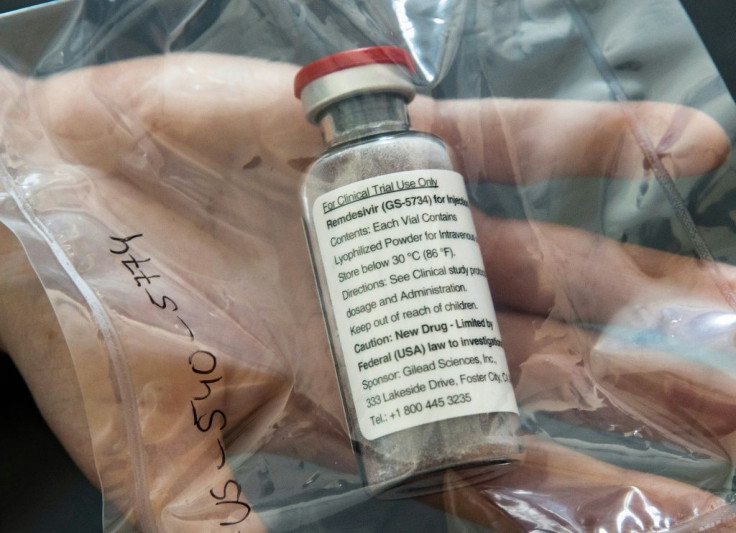
Remdesivir broke onto the world stage when it was given to President Donald J. Trump while he was at Walter Reed National Military Medical Center for treatment of COVID-19. The antiviral drug had been developed by U.S. drug maker Gilead Sciences, in the hopes it would treat viruses like hepatitis, SARS and Ebola. It was never FDA approved.
Then, in May 2020, remdesivir received FDA emergency use authorization (EUA) for treatment of children and adults hospitalized with COVID-19. This EUA was upgraded to any adult or child admitted to the hospital for COVID-19 symptoms, regardless of severity.
NEJM Study
The study published in NEJM on October 8 followed over 1,000 hospitalized patients with COVID-19 who had a lower respiratory tract infection, which would be either pneumonia or bronchitis. The patients were given either remdesivir or a placebo.
The results showed that the patients who received remdesivir recovered within 10 to 11 days, while those who received the placebo were ill for about 15 days.
As with all medications, remdesivir can cause adverse events or side effects, and some can be quite serious. These include changes in kidney function, anemia, respiratory failure, and a rise in blood sugar levels, to name a few.
A total of 131 of the 542 patients who received remdesivir experienced a severe adverse event, but so did 163 of the 516 in the placebo group. The most serious was respiratory failure and the patients required intubation so they could be placed on a ventilator. Less serious adverse events occurred among 273 patients in the remdesivir group and 295 in the placebo group.
However, despite the shortened length of time patients would be ill, the researchers acknowledged that the medication did not affect the death rate. In the conclusion, the authors wrote: “[G]iven high mortality [related to COVID-19] despite the use of remdesivir, it is clear that treatment with an antiviral drug alone is not likely to be sufficient for all patients.”
Related Story: President Trump Receives Remdesivir, But What Is It?
The WHO study
The WHO study, called the SOLIDARITY trial, was given a different goal. The researchers looked at mortality rates among patients with COVID-19 who were given remdesivir. The study authors wanted to know if more people would stay alive on remdesivir.
The researchers recruited over 11,000 patients who received either remdesivir, hydroxychloroquine, lopinavir, interferon and lopinavir, or nothing. Hydroxychloroquine is used to treat or prevent malaria; lopinavir is an antiviral medication used to treat HIV.
The results showed that there were no differences in the rates of death among any of the patient groups. The trials with hydroxychloroquine and the lopinavir trials were discontinued early because here was no proof they were beneficial. And looking at the 2,743 patients who received remdesivir, 11% of them died – about the same number as those who received nothing, at 11.2%.
The take-home
So, what is the non-medical person to take away from this information? On face value, the studies aren’t that different – they both said that remdesivir didn’t make any difference in the number of deaths resulting from COVID-19. But, the first one said that it shortened the course of the illness.
Maybe the decision to use the drug depends on hospital resources and how quickly they can get patients discharged home.
Medical Daily contacted experts for comment. Theywere not available at deadline.
Published by Medicaldaily.com



























