Crohn’s Disease And Ulcerative Colitis Patients May Benefit From Restarting Infliximab Treatment
After over a year of discontinued treatment with the popular immunosuppressant drug Remicade (infliximab), patients with Crohn’s disease and ulcerative colitis may find jumpstarted improvements in their digestive health.
The findings come from a new study published in the journal Clinical Gastroenterology and Hepatology, which analyzed the remission and reaction rates of 128 patients with one of the two major inflammatory bowel diseases. Where prior treatment may have failed or ceased to offer new benefits, waiting a period of roughly 15 months before starting the Remicade regimen could effectively make the drug work overtime.
"Our findings suggest that starting infliximab after a history of prior therapy can be very beneficial to patients," said lead study author Dr. Filip Baert, from the department of gastroenterology, University Hospitals Leuven, in a statement. "Most striking, response to infliximab can be regained in a subset of patients who previously had lost response to the treatment and failed several other treatments thereafter."
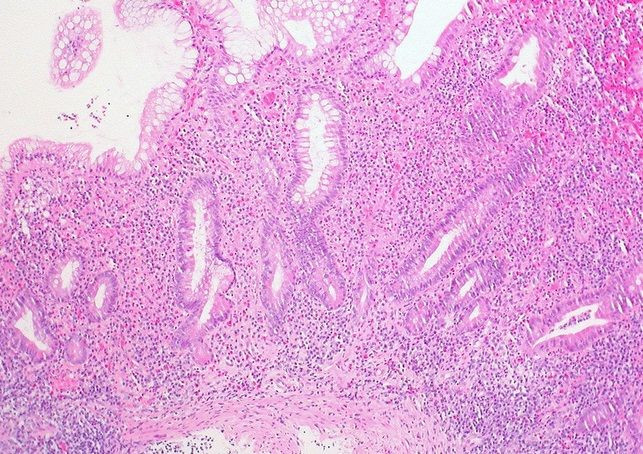
Patients with IBD suffer from abdominal pain and digestive difficulties because the white blood cells rushing to stabilize the patient’s intestines produce an immune response in what is actually a healthy body. As an immunosuppressant, Remicade quiets that response. Unfortunately, the drug isn’t specific enough to keep the rest of the immune system intact, so the whole thing gets weaker.
Worldwide, incidence of IBD hovers around 396 per 100,000 people, or just shy of 29,000,000 in total. Precise data is limited, in part because doctors have yet to agree on a gold standard for diagnosis. What may be consequential inflammation as a result of diet or illness could also indicate a chronic condition, which deserves extensive treatment. In addition, the symptoms of both diseases fall on a spectrum. Toward the mild end is the occasional discomfort and infrequent treatment, while severe cases force people to the floor, immobilizing them, and can demand whole bowel removal.
Of the 128 people reviewed, seven had severe reactions to the Remicade infusions. Those who didn’t respond well were given immunomodulators — separate drugs that also help suppress the immune system, particularly when other methods haven’t worked or the patient is taking an anti-inflammatory corticosteroid.
Subjects who ended their prior treatment in remission showed a 78 percent response rate to the new regimen, and among those who were forced to stop prior treatment, either because it didn’t work, stopped working, or a separate factor compelled them to, 45 percent saw improvements. To the researchers’ minds, this suggested the need for careful pharmacologic monitoring, in the form of blood tests to check the medicine’s presence and any potential antibody response.
"Clinicians understandably have been reluctant to rechallenge patients with infliximab given the fear of immediate or delayed hypersensitivity reactions with dose interruptions,” Baert said. “This study provides the important message that restarting infliximab after a drug holiday is feasible.”
Source: Baert F, Drobne D, Gils A, et al. Early Trough Levels and Antibodies to Infliximab Predict Safety and Success of Reinitiation of Infliximab Therapy. Clinical Gastroenterology and Hepatology. 2014.
Published by Medicaldaily.com



























