Deep Brain Stimulation For Alzheimer’s: Can People With Cognitive Disorder Consent To Treatment?
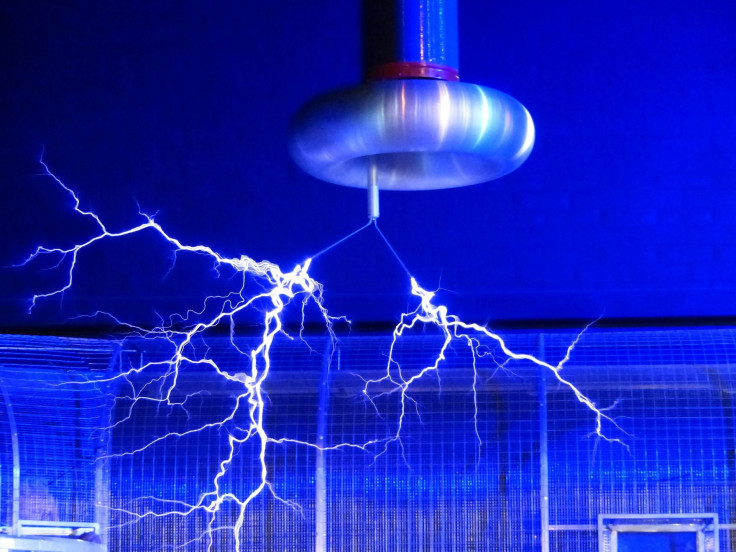
A possible new treatment for Alzheimer’s disease has raised ethical questions because the procedure involves an invasive surgery to implant a device that then electrically stimulates certain parts of the brain.
Deep brain stimulation is already used to treat conditions like Parkinson’s disease, specifically neurological symptoms like tremors, the National Parkinson Foundation explains. The procedure “blocks electrical signal from targeted areas in the brain,” such as those involved in movement.
Read: Concussions Speed Up Alzheimer’s
But Alzheimer’s disease is a type of dementia marked by memory loss and confusion, so experts from the University of Pennsylvania argue it may cause an ethical quandary if the deep brain stimulation is used on those patients in clinical trials, particularly when it comes to informed consent, a process by which a patient permits a doctor to perform a medical treatment — while fully understanding the possible consequences.
The review in the Journal of Alzheimer’s Disease recommends “robust assessment and regular monitoring of subject decision-making.” That would extend to making sure that the people with Alzheimer’s understand the purpose of a clinical trial, during which the “scientific goals will have priority over therapeutic goals.”
According to a statement from Penn Medicine, one suggestion in the journal article is to have an expert who is not affiliated with the trial evaluate the patients’ understanding of the deep brain stimulation procedure and associated risks.
“As the number of people affected by Alzheimer’s continues to grow, along with its substantial costs to individuals, their families, and society, novel therapies are urgently needed,” co-author Dr. Andrew M. Siegel, a clinical psychiatry professor in the Perelman School of Medicine, said in the statement. “However, this enthusiasm should be tempered by prudent ethical considerations to help better protect the patients.”
See also:
Published by Medicaldaily.com



























