Criticism Quickly Follows Remdesivir Approval
Less than 24 hours after the FDA approved remdesivir, the first therapy to treat COVID-19, medical experts are questioning the wisdom behind the move, stating that some trials did not show any efficacy, especially in severe patients. Remdesivir, an anti-viral that keeps the virus from replicating, can induce serious adverse events, including kidney failure and liver damage. At least one case study has been reported of a man treated with remdesivir who developed severe liver injury. Other reports indicate that remdesivir can cause damage to the mitochondria, which supplies the cell with the energy necessary for its biochemical functions.
“Not supportive of this decision at all,” tweeted Eric Topol, MD, director, Scripps Research Translational Institute, soon after the FDA's announcement Thursday evening. “Does it work early? Does it work late? Does it work anytime? So much unresolved."
Peter Bach, MD, director of Memorial Sloan Kettering Cancer Center’s Center for Health Policy and Outcomes, concurred, also in a tweet.
"Agreed, astonishing. Of the three included studies, one lacked control, two lacked blinding, all three lacked inclusion of current standard of care, results mixed, and an entirely negative real world RCT was larger than these put together. 'Effective'? What?"
Scott Gottlieb, MD, former FDA commissioner, had a slightly different opinion. As he said to Squawk Box Friday morning: “We have to be comfortable with singles and doubles when it comes to developing drugs against COVID right now. We rushed a lot of medicines into clinical development, not necessarily optimizing them. This is sort of the first generation of medicines. Nothing, probably, is going to be a home run.”
The Food and Drug Administration, in its approval Thursday evening, said remdesivir is allowed for patients 12 years and over who weigh at least 88 pounds. Remdesivir is only permitted for use in hospitals or other medical care settings that provide inpatient care.
The FDA based its approval decision on the results of three clinical trials. These trials tested remdesivir, which is given by infusion, on patients with different levels of severity and different recovery periods.
One trial tested the drug’s performance on 541 patients with mild, moderate and severe cases. A nearly equal of patients received a placebo. The remdesivir group, overall, took 10 days to either walk out of the hospital or remove their supplemental oxygen. Those who took the placebo took an average of 15 days were able to do the same.
A second trial looked at the drug’s performance in those with moderate diseases after 5 days, and also after 10 days, against standard of care. The drug worked best during the 5-day stretch. Those in the 10-day group fared better than those receiving standard of care, but statistically it wasn’t an important difference.
The third trial was devoted to those with severe disease. The nearly 400 patients were placed in either a 5-day evaluation period, or a 10-day. Again, those in the shorter period of time fared better than those in the longer period;
One large study did not show good outcomes. A World Health Organization study, which looked at mortality rates among those with severe disease, found that those taking remdesivir fared no differently than those patients who had received other treatments or nothing.
Since May hospitals have used remdesivir under an emergency use authorization, but only to treat those hospitalized with severe cases of COVID-19. It was later upgraded in August to include any child or adult admitted with COVID-19 symptoms.
With the new approval, the FDA expanded its use to include any patients, save for younger children, who are hospitalized with the virus. When President Trump was hospitalized with COVID-19 on Oct. 3, one of his treatments was remdesivir.
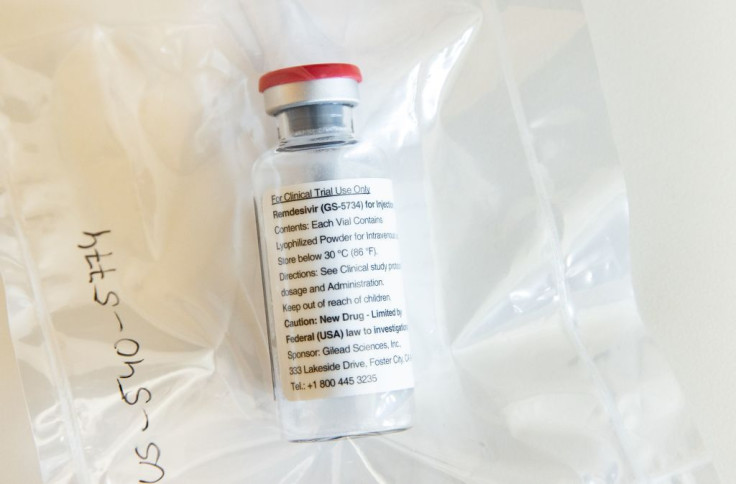
Mr. Trump has long been a supporter of remdesivir, made by the biotech firm Gilead Sciences. He said in late April that he wanted the FDA to move as quickly as it could to approve this anti-viral treatment.
Remdesivir is not a new drug. Gilead Sciences had developed remdesivir to treat viruses like hepatitis, SARS and Ebola. It did not receive approval for these diseases.
For patients with commercial insurance in the US, a course of remdesivir will cost $3,120, or $520 per vial. For those in government healthcare programs, the cost will be $2,340 per course of treatment.
The number of deaths related to COVID-19 continues to rise. As of today, there were more than 223,000 deaths and thousands of new cases across the country. The New York Times reports more than 75,000 cases on October 22, but NBC says it’s even higher – 77,640.
Community spread has contributed to the high of cases and can occur from any type of gathering, no matter how small, One example of community spread was the Sturgis Motorcycle Rally held in August in South Dakota. There were almost 500,000 attendees from all over the country. There was a significant increase in cases in the Dakotas and surrounding states, but cases also reached far beyond.
Public health officials don’t have an accurate count, but they estimate that the rally caused the spread of COVID-19 to more than 330 people in 23 states. One death has been directly linked to the event.
Published by Medicaldaily.com



























