FDA Warnings Are Often Ignored or Misinterpreted
Researchers have broken down the way in which the U.S. Food and Drug Administration notifies the general public and health care providers about unanticipated risks from approved medications into four different categories: warnings about serious harmful events, recommendations against use in certain patient populations, averting harmful drug-drug interaction, and calls for increased lab or clinical monitoring, according to a study published Thursday.
Researchers said that the impact of these FDA warnings and alerts have been “varied and unpredictable” and the most effective notices were those four were public warnings about potential serious adverse effects of a certain drug, but even these alerts varied in their impact.
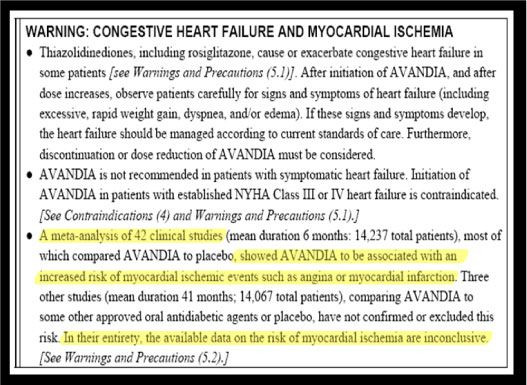
The study examined 1,432 articles published in the last two decades that assessed the impact of FDA warnings and found that several studies found that many patients stopped taking the diabetes drug rosiglitazone after an FDA alert noted an increased risk of cardiovascular events in people taking this drug, and led to decreased use of rosiglitazone and increased use of other less risky diabetes treatments.
However, a similar 2010 FDA warning for asthma patients that said that long-acting beta agonists should not be used without an asthma controller medication like inhaled corticosteroids had little effect. The rates of controller medication use along with long-acting beta agonists were low before FDA issued the warning, and barely increased after the advisory was released.
Researchers also pointed out that although FDA warnings that recommended against specific groups of patients to avoid certain medications sometimes decreased use, it also produced unintended consequences. When FDA issued warnings about the use of antidepressants among children and adolescents, it resulted in significant decreased use of these medications by adults as well as children. Previous studies found that the warning may have coincided with an unexpected increase in suicides among children and adolescents due to increases in untreated depression.
Warnings about harmful drug and drug interactions had some impact, but reductions in co-prescribing were usually observed only after repeated FDA risk advisories that took take up to years. The initial warnings on the use of cisapride with contraindicated products were first sent in February 1995, but significant changes in cisapride co-prescribing were not seen until after the third alert in June 1998.
Researchers said that recommendations to increase clinical or laboratory monitoring for patients taking certain drugs generally produced “no evidence of a large or sustained impact of the FDA recommendations”. When the FDA issued an advisory to monitor patients using antipsychotic medications for hyperlipidemia and diabetes, there were no increases in glucose testing following the administration’s warning.
Researchers said that although some communication efforts were strong and produced an immediate effect, many had little or no impact and even led to unintended harmful consequences.
"Communicating risk to large groups of people is a complex science," said study director Caleb Alexander, associate professor of medicine at the University of Chicago. "But success or failure at this can have significant consequences. As such efforts become more and more common — with the FDA's mandate to establish a more active surveillance system — we will need a better understanding of how to make them work and where they can go wrong. And we need more and better studies of the successes and failures of this process."
The most successful communications were those that were simple, specific, had alternatives available and were reinforced over time, the researchers concluded.
The study is published in the journal Medical Care.
Published by Medicaldaily.com



























