GlaxoSmithKline Cancer Vaccine For Stage 3 Melanoma Fails In Late Trials, Experimental Research Continues
GlaxoSmithKline (GSK) announced that its experimental vaccine for treating patients with stage 3B/C melanoma failed in a Phase 3 clinical trial. Although no safety concerns exist, the therapeutic vaccine failed to meet its first of two key endpoints — significantly extending disease-free survival in the study population. The company will continue with the trial to see if the second endpoint, which is to discover a subset of patients who may be helped by the vaccine, is reached.
“We want to thank all patients, their families and healthcare workers for their involvement in the trial and we remain committed to identifying a patient sub-population who may benefit from this investigational treatment,” Vincent Brichard, senior vice president of GSK Vaccines, stated in a press release. GlaxoSmithKline focuses on pharmaceuticals, vaccines, and consumer healthcare; based in the United Kingdom, the company has a global reach with offices in more than 115 countries.
The vaccine is intended for stage 3B/C melanoma patients with macroscopic nodal disease whose tumors, though removed surgically, have been found to express the MAGE-A3 gene. MAGE-A3 is an antigen expressed in about 65 percent of stage 3 melanomas (and a variety of other cancers), with no presentation in normal cells.
The Independent Data Monitoring Committee, which was established by the European Organization for Research and Treatment of Cancer to review the status of clinical trials, unanimously recommended that GSK continue the trial until the second co-primary endpoint can be assessed. Results are expected in 2015. In the meantime, GSK continues to evaluate the same experimental vaccine in a separate Phase 3 study of non-small cell lung cancer patients after surgical removal of the primary tumor. Data from this trial is anticipated in the first half of 2014.
Cancer Vaccines
The National Institutes of Health explains that cancer vaccines fall within a category known as ‘biological response modifiers,’ which stimulate or in some cases restore the immune system and so strengthen the body’s ability to fight infection and disease. Cancer vaccines may be either prophylactic or therapeutic. Prophylactic vaccines are intended to prevent cancer from developing in healthy people while therapeutic vaccines are intended to treat an existing cancer by strengthening the body’s immune system against the cancer.
One of the greatest difficulties for scientists is trying to prevent cancer from returning. Simply boosting the immune system in natural ways does not always work. If cancer were a thief, then sometimes it acts like a friend with a key — not seen as an intruder, it knows how to ‘get in,’ so to speak, and can bypass a strong immune system. What is needed is a reactivation of the immune system so that the body recognizes cancer as a threat.
Several types of cancer vaccines, described by the American Cancer Society, are currently being studied.
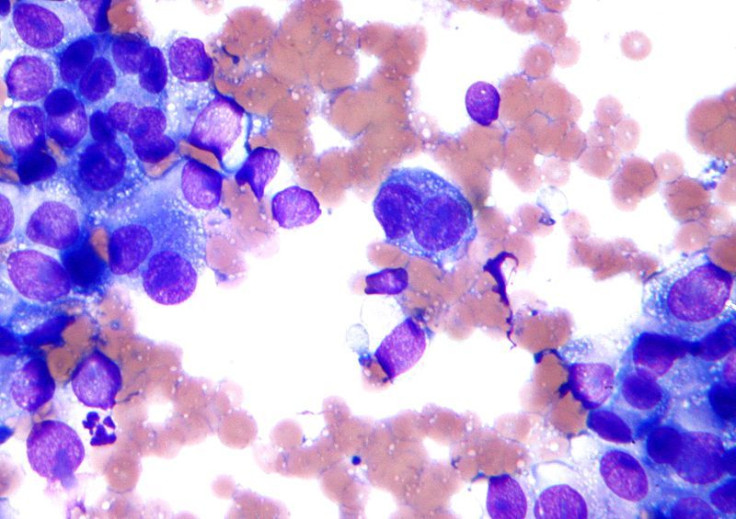
Tumor cell vaccines are made from actual cancer cells that have been removed during surgery, and are then treated in a lab so that they cannot form more tumors. Further treatments make them unrecognizable to the immune system so that when they are injected back into the patient, the immune system begins to attack similar cells that may still be in the body.
Antigen vaccines work to boost the immune system in a similar way but they only use one or a few antigens from the tumor cells rather than the whole tumor cell.
Dendritic cell vaccines are based on special immune cells within the body’s system that can recognize cancer cells and then break them down in ways that make it possible for other immune cells (T cells) to attack them.
DNA vaccines are based on the fact that the immune system may need further stimulation than what tumor cell vaccines or antigen vaccines may provide. As a way to induce a steady supply of antigens to keep the body’s defense system responding, these vaccines activate DNA that instructs the cells to produce antigens, and this ultimately provokes the body’s response.
Source: National Cancer Institute Fact Sheet. Cancer Vaccines. 2011.



























