Group B Strep: Get Tested To Save Your Baby's Life
Group B streptococcus (GBS) is designated by the Centers for Disease Control and Prevention (CDC) as the number one killer of newborns in the U.S.
Group B strep is caused by a type of bacteria that normally lives in the intestine, vagina, or rectal areas, and it is found in anywhere from 15 to 40 percent of all healthy adult women. Anyone can carry GBS and those who do are not unclean. Women who do test positive for GBS are said to be 'colonized.' Group B strep colonization is not a sexually transmitted disease, and for most women, there are no symptoms of carrying the GBS bacteria.
A mother who is colonized can pass GBS to her baby during delivery; acquisition by an infant born to a colonized mother occurs in 29 to 72 percent of cases. It is important to note that not every baby born to a mother who tests positive for GBS will become ill.
How do I know if I have it?
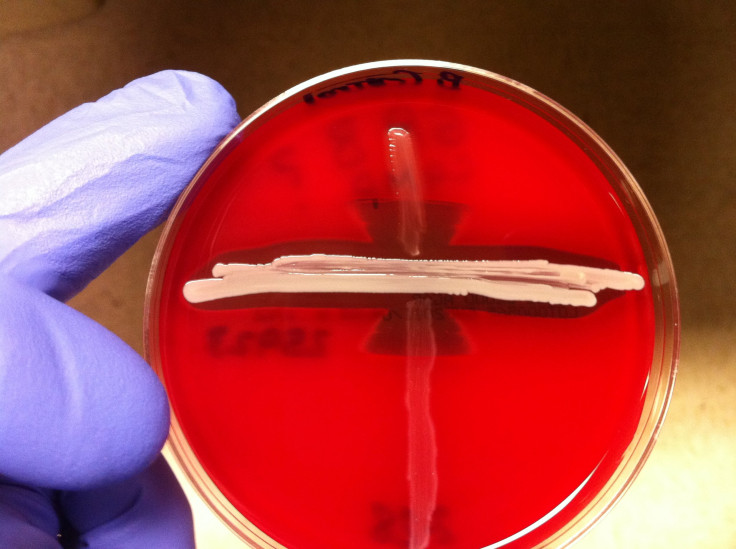
CDC's guidelines recommend that a pregnant woman be tested for Group B Strep when she is 35 to 37 weeks pregnant. The test involves a swab of both the vagina and the rectum. After the sample is taken to the laboratory, a culture is analyzed for any presence of GBS. Test results are usually available within 24 to 48 hours.
Although GBS is rare in pregnant women, the outcome can be severe, and therefore physicians include testing as a routine part of prenatal care. In fact, the American Academy of Pediatrics recommends that all women undergoing labor who have risk factors prior to being screened (for example, women who have preterm births before the 35th week) are automatically treated with IV antibiotics until their GBS status is established.
A woman who tests positive for GBS and receives antibiotics during labor has a one in 4,000 possibility — compared to a one in 200 possibility if she does not receive antibiotics during labor — of delivering a baby with group B strep disease. Antibiotics before labor starts are not an effective way to get rid of group B strep bacteria since they naturally live in the gastrointestinal tract and the bacteria may return. Oddly, a woman may test positive at certain times and then not at others; for this reason it is important to be tested between 35 and 37 weeks of pregnancy.
The American Pregnancy Association recommends that pregnant women who had a baby with GBS disease in the past and those who have had a urinary tract infection during pregnancy caused by GBS be treated with antibiotics during labor.
What about my baby?
Babies may experience prenatal, early, or late-onset of GBS. Prenatal onset of GBS occurs before the baby is born, early onset occurs from birth to seven days old, and late onset occurs from seven days to three months old. In rare cases, onset may occur later than three months, but the typical timeline for GBS to infect a baby is within three months.
Signs and symptoms of prenatal onset GBS include decreased fetal movement or no movement after 20 weeks. Sometimes an unexplained fever in the mother signals her unborn child's infection status.
The signs and symptoms of early onset GBS include:
- Breathing problems, heart and blood pressure instability
- Gastrointestinal and kidney problems
- Sepsis, pneumonia, and meningitis are the most common complications
According to the CDC, the most common symptom of late-onset GBS include meningitis. Late-onset of GBS, more rare than early onset, may be a result of either delivery or coming into contact with someone with the bacteria. Babies with early-onset are treated the same as their mothers would be, which is through intravenous antibiotics.
A mother whose child died of late onset GBS lists these symptoms:
- High-pitched cry, shrill moaning, whimpering
- Marked irritability, inconsolable crying
- Constant grunting as if constipated
- Projectile vomiting
- Feeds poorly or refuses to eat, not waking for feedings
- Sleeping too much, difficulty being aroused
- High or low or unstable temperature; hands and feet may still feel cold even with a fever
- Blotchy, red, or tender skin
- Blue, gray, or pale skin due to lack of oxygen
- Fast, slow, or difficult breathing
- Body stiffening, uncontrollable jerking
- Listless, floppy, or not moving an arm or leg
- Tense or bulgy spot on top of head
- Blank stare
- Infection at base of umbilical cord or in puncture on head from internal fetal monitor
Prevention
Unfortunately, there is no group B strep vaccine available, although researchers are working toward developing one. Birth canal washes with the disinfectant chlorhexidine do not reduce transmission of GBS bacteria or avert all possibility of a baby contracting early-onset disease. Intravenous antibiotics during labor are the only proven strategy to protect a baby from early-onset GBS disease.
July is International Group B Strep Awareness Month. The one preventative measure within everyone's grasp is knowledge and the dissemination of knowledge. A mother-to-be need only to begin a conversation with her obstetrician, while those who love her need only to encourage her to do so.
Source: Baker CJ. Streptococcal Infections: Clinical Aspects, Microbiology, and Molecular. Oxford University Press. 2000.
Published by Medicaldaily.com



























