Healthcare Inequality Grows Between States: Find Out Your State's Ranking
While gaps in healthcare access between the rich and poor families in America have long been discussed, a new report from the Commonwealth Fund shows a more nuanced soure of inequality. Another gap in healthcare exists based on geography, in which low-income residents of high-performing states are more likely to receive care than high-income residents elsewhere.
In a study titled “Healthcare in the Two Americas,” researchers from the Commonwealth Fund rated the quality of healthcare for low-income Americans in the 50 states and the District of Columbia. They analyzed several measures of prevention and quality, health outcomes, access, and potentially avoidable hospital use.
“There are often two Americas when it comes to healthcare, divided by geography and income,” the study authors write.
Hawaii, Wisconsin, Vermont, Minnesota, and Massachusetts were found to have the best performing health systems for low-income populations, in that order. On the other end of the spectrum, Southern states dominated the bottom of the list, with Arkansas, Alabama, Louisiana, Oklahoma, and Mississippi, in last place.
For instance, a poor resident of Vermont is more likely to have a regular source of primary care than a rich person living in Montana, a state that performed worse in healthcare access. A low-income person living in Nevada is less likely to be obese than a high-income resident of Louisiana. A low-income child in Florida, which ranked 43rd in the list of 51, is twice as likely to be uninsured compared to a low-income child in New York, a state that ranked 17th.
If all states adopted the healthcare standards held by the highest-performing states, an estimated 86,000 people fewer people would die prematurely and 30 million more people would be insured. For a more concrete example, if Florida were to reduce its 8.5 percent infant mortality rate to California’s 5.5 percent, 1,101 fewer infants would die before their first birthday. Furthermore, if Florida dropped the proportion of uninsured low-income adults from its current 48 percent to Massachusetts' 12 percent, over 1.5 million more adults would be insured.
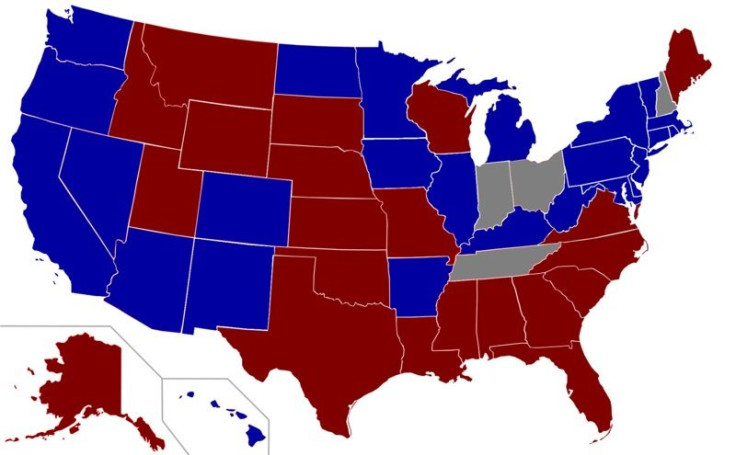
Although the Affordable Care Act was designed to address these inequalities, its implementation in reality will likely exacerbate the disparities. The 26 states that rejected the expansion of Medicaid eligibility to insure millions more Americans also happen to be among the worst-performing states.
To see how your state performed, view the interactive map below.
Highest-Performing States: Top 10
- Hawaii
- Wisconsin
- Vermont
- Minnesota
- Massachusetts
- Connecticut
- Rhode Island
- South Dakota
- Iowa
- Maine
Lowest-Performing States: Bottom 10
41. West Virginia
43. Florida
44. Missouri
45. Georgia
46. Kentucky
47. Arkansas
48. Alabama
49. Louisiana
49. Oklahoma
51. Mississippi
Published by Medicaldaily.com



























