History Of Medicine: The Unknown Netherworld Of Anesthesia

States of altered consciousness have long fascinated philosophers, junkies, and priestesses, yet the complete loss of consciousness is not considered to be either rarified or impressive. By way of anesthesia, nearly 250 million people each year “go under” during one or another medical procedure. What is remarkable in this is that these everyday drugs remain utterly mysterious to the scientists who develop and use them.
“We still don’t know how they work,” Dr. Roderic G. Eckenhoff, a professor in the Department of Anesthesiology and Critical Care at the University of Pennsylvania, told Medical Daily.
Among the most original hypotheses in currency today is that of Dr. Luca Turin of the Alexander Fleming Research Center in Athens, Greece. Rather than through more conventional pharmacological mechanisms, general anesthetics “perturb electron currents in cells” and so extinguish consciousness by subtly changing the electronic state of proteins, Turin believes. His theory reaches far beyond the two more common though still quite controversial schools of thought.
On one side of the divide, scientists believe anesthetics work by interacting with a few key ion channels that regulate synaptic transmission and membrane potentials in the brain and spinal cord. On the other side, researchers including Eckenhoff, theorize anesthetics interact with dozens, maybe even hundreds of molecular targets to produce their effects. The authors of “Consciousness and Anesthesia,” which appeared in Science in 2009, suggest that agents of anesthesia target, either directly or indirectly, a “posterior lateral corticothalamic complex centered around the inferior parietal lobe, and perhaps a medial cortical core.” Unconsciousness results, then, when anesthetics “deactivate” the posterior corticothalamic complex, yet also because they produce what the authors describe as “a functional disconnection” between subregions of this complex.
“Anesthetics also tend to have a certain physical-chemical profile,” Eckenhoff explains, noting how they are, for the most part, uniformly small, uncharged molecules. While the blood brain barrier is able to filter out other drugs, the unique qualities of an anesthetic molecule allow it to slip past this guard. “It’s like the blood-brain barrier doesn’t even exist,” he says.
This much, then, may be common knowledge today, but there were many years when even less was known about these drugs.
Brief History
Western historians point to the 18th century as the beginning of the modern age of anesthesia. However, since recorded time, scientists have been experimenting with plants and other herbal remedies to produce the necessary effects of immobilization and loss of consciousness. While various ancient civilizations discovered one form or another, the Chinese doctor Bian Que notably created his own toxic drink for use during surgical procedures as far back as 300 B.C. In Europe, an Italian physician, Theodoric of Lucca, reportedly soaked sponges in opium and mandragora to relieve the pain of patients undergoing operations during the 13th Century. And less than 200 years later, Paracelsus, the Swiss German physician and Renaissance man who found the discipline of Toxicology, began using ether on animals.
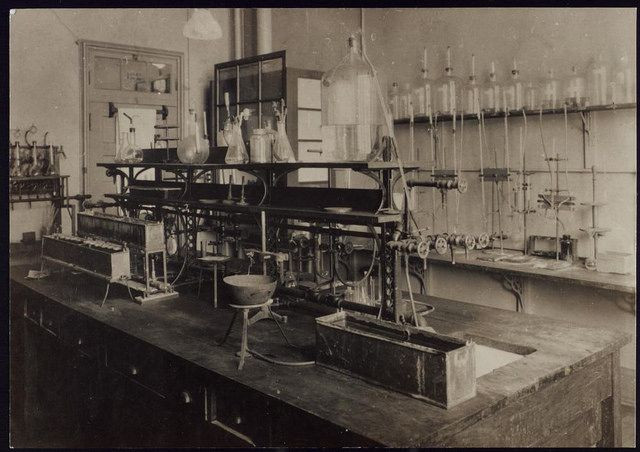
Still, a safe, effective, and most importantly consistent anesthesia did not emerge for some years. According to Eckenhoff, who is no stranger to the lab, “Empiricism and trial and error has characterized most of anesthetic discovery,” and this is evidenced in most accounts.
English scientist and Unitarian minister Joseph Priestley is given credit for isolating nitrous oxide around 1774. He believed someday his research on gases and the application of “airs” would be of great medicinal use. Thomas Beddoes, the physician, continued his work with his own explorations into the potential medical uses of gases during the late 1780s. He founded the Pneumatic Institute in England during 1798 and there, Peter Mark Roget, of Thesaurus fame, worked with him and Humphry Davy, author of Researches, Chemical and Philosophical: Chiefly Concerning Nitrous Oxide, or Dephlogisticated Nitrous Air, and its Respiration, on nitrous oxide (laughing gas) research. Through “auto-experimentation,” these intrepid souls learned the effects of various gases on their own human bodies.
However, it was not until several decades later that the gas was used for the first time in clinical practice. That credit belongs to Dr. Crawford Long who in 1842 administered ether anesthesia during a surgery to remove a tumor. From here, the science advanced in fits and starts.
In 1846, William Morton publicly demonstrated the power of gas in the operating theatre of Massachussetts General Hospital. For about three minutes a patient breathed ether vapor through Morton’s simple apparatus and then "sank into a state of insensibility," according to accounts written at the time. Following this sensation, reports from Europe begin to emerge of doctors and surgeons using nitrous oxide, chloroform, and even cocaine to fully or locally anesthetize patients during operations and procedures.
Around the same time, techniques for administering the gases become refined; the face mask is designed, eventually flow meters and vaporizers are developed to modulate the gas.
Around the turn of the century, experiments using anesthesia during childbirth begin. In 1934, Ralph M. Waters in Wisconsin sedates a man with thiopental for the first time. A couple of decades later the first medical journal devoted to anesthesiology is published, speeding news of advancements throughout the field. In 1951, Halothane is synthesized, followed by Propofol in 1977. Shortly thereafter, Ondansetron, Vecuronium, and Sevoflurane are approved by the FDA and enter clinical practice.
And then the car appears to stall, rolling to a complete stop. “We haven’t had a new anesthetic in at least 40 years,” says Eckenhoff.
Future Focus
Why the recent lack of innovation? Apparently, the current generation of anesthetics work well enough for most. “We don’t kill too many people,” Eckenhoff jokes. “It’s a pretty safe speciality and a pretty safe experience.” Since developing new drugs is a highly expensive practice, the pharmaceutical industry doesn’t feel any great need (or pressure) to conduct research in this area.
However, Pharma might want to rethink its "why fix what isn't broken'" stance. First, there are acute side effects, including respiratory depression, which can lead to death. Though this only happens in admittedly rare cases — Michael Jackson is an example of such an anesthesia-related death — it now may be possible to modify the molecules and make them safer with a little help provided by the latest advances in medicine and technology.
A second good reason to pursue new anesthesia drug development is that researchers have begun to appreciate the chronic effects of these drugs. In fact, many scientists believe anesthetics do not leave the brain unchanged. New data suggest children who have been exposed to these drugs multiple times while under the age of 4 develop learning disabilities. And animal research has proposed that anesthetic drugs may accelerate the development and progression of Alzheimer’s disease.
Though not yet conclusively proven, these possible long-term side effects are a serious concern. After all, anesthesia is being used more frequently today and for a wider range of procedures, including diagnostic tests such as colonoscopies and invasive radiology. "We’re pulled all over the hospital to participate in procedural care, everywhere," says Eckenhoff.
With Pharma not yet interested, it might fall to academia — or a few fearless biohackers — to return to the lab and investigate the still unknown, possibly forever unknowable territory of induced unconsciousness. A new generation of anesthesia awaits discovery.



























