HIV Medication Delivered Through Dissolvable Fabric Could Provide Faster Protection
A new dissolvable fabric could pave the way for faster, more efficient delivery of the HIV medicine, maraviroc. Published in the journal Antimicrobial Agents and Chemotherapy, the study suggests a method of HIV protection that avoids messy gels or cream, with the added benefit of stronger potency.
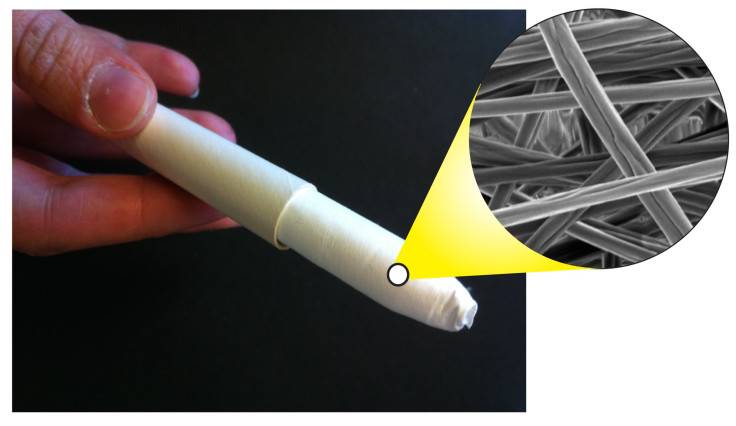
Bioengineering researchers from the University of Washington have developed the new fabric from dissolved polymer, through which they ran an electric current, and spun the resulting string around a grounded surface. The end product is a patch of fabric women can apply just as they would a tampon, before engaging in sex, to prevent the infection of HIV.
“This could offer women a potentially more effective, discreet way to protect themselves from HIV infection,” said Cameron Ball, a UW doctoral student in bioengineering and lead author, in a statement. The trouble with current options, Ball explains, is their balance of timeliness and discreetness. Oral pills, while offering the benefit of quick ingestion, need time to travel throughout the body. Topical agents, meanwhile, are direct yet disruptive.
“The effectiveness of an anti-HIV topical drug depends partially on high-enough dosages and quick release,” Ball said. “We have achieved higher drug loading in our material such that you wouldn’t need to insert a large amount of these fibers to deliver enough of the drug to be helpful.”
Typical anti-HIV medicines contain a three percent solution relative to the rest of the product’s total mass. The new fabric contains a 30 percent solution, and because of how the fibers were designed, the researchers say, no matter how much of the drug was in the fabric, the dissolve time remained a constant six minutes. The fabric could be applied via traditional cardboard applicators or formed into an intravaginal ring, similar to those used for contraception.
Maraviroc isn’t the only medicine the fabric can tolerate. Lead researcher of the study, associate professor of bioengineering Dr. Kim Woodrow, said the goal for the fabric is to accommodate multiple drugs. “We think the fiber platform technology has the capability of being developed into multifunctional medical fabrics that address simultaneously challenges related to biological efficacy and user preferences,” she explained.
Woodrow and her team created the fibers using a polymer base, which they combined with maraviroc and other ingredients that help to make the end product more water soluble and dissolve quicker. A high-voltage generator then charges the syrupy substance before it gets shot through a syringe. This process turns the substance into a long string, to be wrapped around an electrically grounded surface. Within five minutes’ time, these fibers get woven into a palm-sized patch of fabric.
The findings build upon prior research that showed fiber materials can hold up to 10 times the concentration of medicine as typical gels and deliver that medicine using a far more effective method. According to the Centers for Disease Control and Prevention, roughly one in four HIV patients is female. In the U.S. alone, this equates to nearly a quarter of a million women living with HIV, 16 percent of whom may not even know they carry the virus.
Source: Ball C, Woodrow K. Electrospun Solid Dispersions of Maraviroc for Rapid Intravaginal Preexposure Prophylaxis of HIV. Antimicrobial Agents and Chemotherapy. 2014.
Published by Medicaldaily.com



























