Huntington's Disease Breakthrough: Scientists Convert Skin Cells To Brain Cells
In a breakthrough discovery, scientists have found a way to convert human skin cells into a specific type of brain cell that becomes degenerate in people suffering from the fatal neurodegenerative Huntington's disease. This method scores over numerous other techniques of specialized cell production, since it does not involve the stem cell stage, and thus avoids production of multiple cell types.
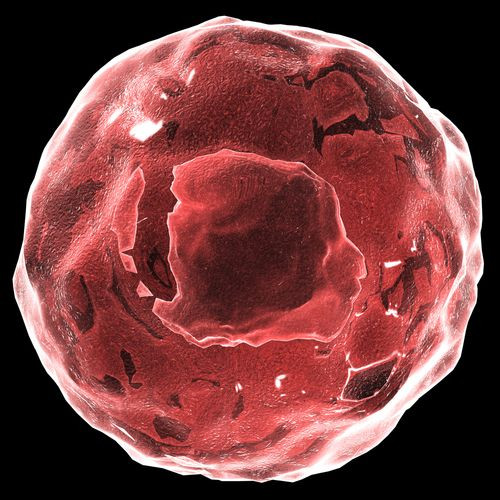
Huntington's is an inherited disease that causes gradual damage to the nerve cells in the brain. Over time, the nerves get completely useless, which leads to loss of function of these areas of the brain. This can affect movement, cognition, and behavior. A nerve cell related to movement that gets affected by this condition is the medium spiny neuron.
Scientists developed these cells from skin cells and injected them into the brains of mice with Huntington's. They were surprised by the results.
"Not only did these transplanted cells survive in the mouse brain, they showed functional properties similar to those of native cells," said senior author Andrew S. Yoo in a statement. "These cells are known to extend projections into certain brain regions. And we found the human transplanted cells also connected to these distant targets in the mouse brain. That's a landmark point about this paper."
In their paper, published in the journal Neuron, the investigators state they used adult human skin cells instead of the commonly used mouse cells or early stage human cells.
But how did the skin cells turn into brain cells? Each kind of cell contains information on how to be another type of cell, though this information may not be used at all. For example, skin cells contain DNA information on how to be brain cells, and this information is tightly packed away.
The scientists wanted to coax the skin cells to use this information. To do this, they first grew the cells in an environment that closely resembled those of brain cells. They then exposed the skin cells to two microRNAs, called miR-9 and miR-124, that altered the DNA packaging and unravelled packaged sections of DNA important for brain cells, allowing expression of genes governing development and function of neurons.
But exposure to the microRNAs alone would result in development of different types of neurons. In order to guide the cells to turn into specific medium spiny neurons, the scientists unleashed additional molecules called transcription factors.
"We think that the microRNAs are really doing the heavy lifting," said co-first author Matheus B. Victo. "They are priming the skin cells to become neurons. The transcription factors we add then guide the skin cells to become a specific subtype, in this case medium spiny neurons. We think we could produce different types of neurons by switching out different transcription factors."
In other words, without the microRNAs this conversion was not possible. The researchers also tested to confirm if the newly formed cells did indeed mimic brain cells. The tests showed that the converted cells expressed genes specific to native human medium spiny neurons and did not express genes for other types of neurons.
The advantage of this technique is that by using the patient’s own skin cells the chances of immune rejection are severely reduced, say the researchers.
Source: Yoo AS, Victor MB, Richner M, et al. Cell. 2014.
Published by Medicaldaily.com



























