Ineffectiveness of Cancer Drugs May Be due to Healthy Surrounding Cells
Researchers and doctors have consistently been baffled by cancer cases in which treatments conducted kill the cancer cells in the laboratory, but provide only partial results in patients, with the cancer returning in as little as a few months. The answers do not lie in the cancer cells themselves, but in the healthy cells in the environment next to them.
A study conducted by the Broad Institute, Dana-Farber Cancer Institute, and Massachusetts General Hospital, researchers studied cells in two different wells – tiny test tubes no larger than a pencil eraser. In the first were cancer cells. In the other were cancer cells mixed with healthy ones. Both cultures were treated with anti-cancer drugs. In the well with only cancer cells, all of cancerous cells died. But in the cultures mixed with healthy cells, the cancer cells developed a resistance to more than half of the 23 agents tested.
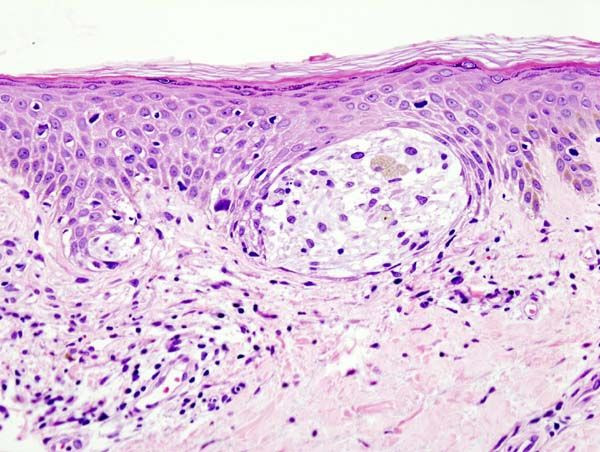
These findings reflect what doctors have seen in cancers such as melanoma. Treatments tend to target certain, commonly malignant genes in tumors known commonly as BRAFs, and are preferred to chemotherapy because of the avoidance of many side effects. In some patients, treatments are overwhelmingly successful and cause melanoma to disappear altogether. In other patients, treatments caused tumors to shrink only slightly in size. These reactions indicate an innate resistance and immunity to treatments. Researchers believe that cancer cells use proteins from surrounding healthy cells to build up a resistance.
Researchers decided to target melanoma, in part because there already exists a targeted therapy for the cancer, in their study. They measured more than 500 secreted factors and found that the one most closely linked with BRAF drug resistance was hepatocyte growth factor (HGF).
Several HGF-inhibitors are already in clinical development or are Food and Drug Administration-approved for other conditions. Another team that studied the same subject in San Francisco came to the same conclusion.
The findings were published in Nature.
Published by Medicaldaily.com



























