Kidney Harvested From Aborted Human Fetus Grown In Rat: An End To Organ Donor Shortage, Scientists Say
In a new study, scientists debut a technique for growing a human kidney, obtained from an aborted human fetus, inside a rat. This new rat model would be “perfect” for drug testing “because the animals are smaller and cheaper, making them scalable for pharmacological testing,” Eugene Gu, an author of the published study, tells Medical Daily in an email.
“Our long-term goal is indeed to have these organs ready for transplant into human patients. However, that would require a large animal model such as a pig rather than a rat.” The video below explains this process:
A fourth year medical student at Duke University School of Medicine, Gu also is a co-founder and CEO of Ganogen, a company located in Redwood City, Calif. A tagline on the company’s website reads Ending the organ donor shortage. While this may appear a noble and worthy goal, the current kidney research, which was sponsored by Ganogen, undoubtedly will raise a red flag or two for many people. However, Gu defends his work, in part, by noting it is subsidized by family, friends, and small investors.
“We feel that our research is more palatable than all the other researchers who use taxpayer money to fund their research involving aborted human fetal tissues, which is the vast majority of major biomedical research labs,” Gu tells Medical Daily. In fact, Gu and his research team acquired the fetal kidneys used in their experiments from Stem Express, a self-described “multi-million dollar company that supplies human blood, tissue products, primary cells, and other clinical specimens to biomedical researchers around the world.”
Experiment & Ethics
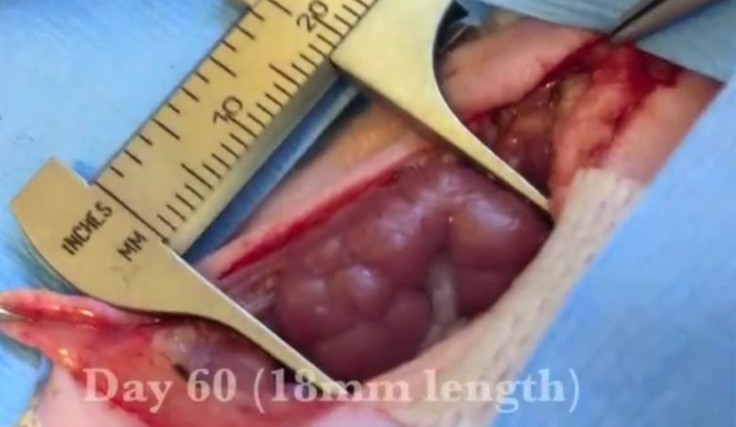
Having obtained the kidney, the researchers transplanted it into an adult rat, connecting the organ via microsurgical techniques to the animals’ blood vessels. Then they adjusted the blood pressure to match. It was this final step of the specialized surgical procedure that spelled success. Past experiments failed when the researchers did not account for the fact that the blood pressure of rats is three times higher than in human fetuses.
“We did this study in rats as proof-of-concept to show that human fetal organs can indeed survive in an animal host, can function to keep the animal alive, and can grow larger over time,” Gu says. Indeed: the rats survived roughly four months after the transplant, and one even lived for 10 months.
Among the ethical questions raised by Gu's work is whether the use of human fetal organs in research should be permissible and whether it is right to transplant human organs into animals. The Ganogen website argues that, as personalized medicine advances and becomes increasingly prevalent, “the differences between mice and men can no longer be ignored.” The reason? Simple animal testing of new drugs, which increasingly target highly specific proteins or genetic variations, cannot sufficiently safeguard our human health. The drug Herceptin is their case in point. This commonly prescribed breast cancer drug caused heart failure in some patients after extensive animal testing proved it safe.
“Our in vivo human organ models may catch and identify human-specific drug toxicities before patients are harmed during clinical trials,” the Ganogen website reads.
Addressing his use of harvested organs from aborted fetuses, Gu says he and his colleagues “do not want to encourage abortions in any way, shape, or form. … If the organs are available, it is better to use them to save somebody's life rather than throw them into the trash bin.” Undoubtedly, Gu's argument is probably echoed in many research labs around the world. That said, most people would still find the details of his work unsavory... unless of course they needed a kidney.
Source: Chang NK, Gu J, Gu S, et al. Arterial Flow Regulator Enables Transplantation and Growth of Human Fetal Kidneys in Rats. American Journal of Transplantation. 2015.



























