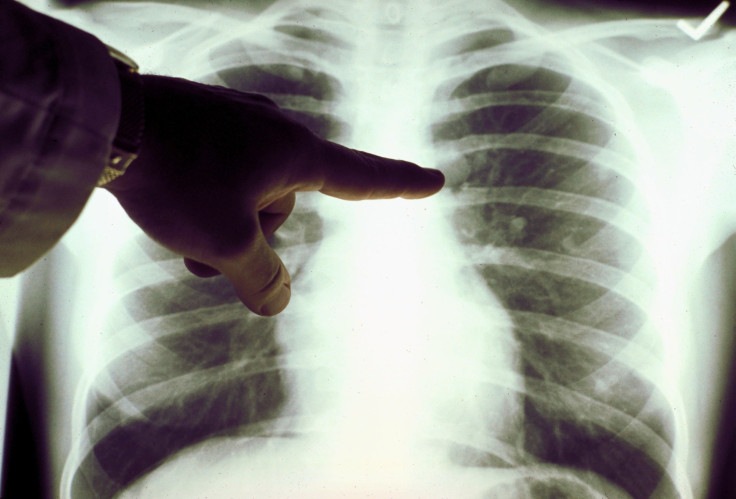
Lung Cancer Breathalyzer In UK Clinical Trials
breathalyzer designed to detect the early signs of lung cancer is undergoing clinical trials at 17 British hospitals, with the aim of having the non-invasive technology in clinics in 2017.
Cambridge-based Owlstone Medical has developed a microchip sensor technology to measure the volatile organic compounds (VOCs) in patients' exhaled breath. Breath testing is already a recognized method for linking specific VOCs in exhaled breath to a certain medical conditions, but current techniques are often expensive, slow and complex to use.
Co-founder and CEO of Owlstone Medical Billy Boyle said their device is much smaller and cheaper than existing technologies; potentially making it a viable tool for doctor's surgeries.
"Historically chemical analyzers take up half the size of a room and cost half a million dollars. So what we've been able to do is use microchip technology to shrink it down from these massive devices to something about the size of a button. And once it's in that form factor, you can build it directly into these disease breathalyzer technologies," Boyle told Reuters.
Boyle said their sensors were originally developed for detecting explosives and toxic gases but were re-programmed to identify the chemical markers of diseases, with a lung cancer breathalyzer the first to reach clinical trial.
Lung cancer kills about 1.5 million people a year, according to the World Health Organization, and is the leading cause of cancer death across the world. Only about 10 percent of patients live more than 5 years, in part because the disease is usually diagnosed too late.
However, the chemical markers of lung cancer are present even in the earliest stage of the disease. Owlstone Medical says their breathalyzer can pick out these minute traces of cancer, meaning current treatments can be administered with a much greater chance of successfully curing the disease.
Boyle said that if the disease is detected early existing treatments work more effectively.
"The challenge is most people present when it's very late stage, and it's about managing symptoms as opposed to curing them. So the key thing that you can do is detect the disease early; and that's what we think the breathalyzer technology allows for," he said.
Developed over 10 years with 28 million dollars (USD) of investment, the device can detect and identify multiple chemicals in a gas flow at very low concentrations, typically parts per billion. Patients wear a breathalyzer mask and breathe normally for several minutes while the sample is collected.
Dr. Robert Rintoul, from Papworth Hospital in Cambridge, where one of the devices is undergoing clinical trials, said the quick, non-invasive breathalyzer could be an important tool for doctors to help determine if high risk patients should be referred for testing in hospital.
"If you have a lung cancer inside your lung, that cancer is producing a range of chemicals in very, very minute amounts. And this device can collect those samples, those tiny amounts of volatile organic compounds, which we can then analyze in the laboratory. And in effect, it's a bit like a fingerprint. If you have a lung cancer we believe that we can detect these samples and that fingerprint will tell us whether the person has lung cancer or not," said Rintoul.
The breathalyzer is also being tested at 16 other hospitals, the largest trial of this type ever conducted.
The clinical study will involve up to 3,000 people who are due to have a biopsy because there is a concern that they may have lung cancer. Prior to having the biopsy, breath samples will be collected from the patients. Once the results of the biopsy are known, doctors will be able to validate the chemical markers they detected in the breath as being lung cancer.
"We've now started putting this into clinics so patients who are coming through and getting other types of tests can provide a breath sample so you can match the two; the tests that are currently used today with what you pick up in the breath. And at the end of that process you have a clinical trial result which means you can start to use it in clinic," said Boyle.
He added that their sensors could one day be used directly by patients if the technology was adapted into a handheld device or built in to a user's smart phone.
"The chip today is already incredibly small, so it's not that hard to envisage how you could put it not only into GP's surgeries, but also into other places where sensor technology can be used directly by patients, by consumers - so they can take control of their own health data and their own health destiny."
In the UK there are about 45,000 new cases of lung cancer each year, costing the Nation Health Service (NHS) 2.5 billion pounds ($3.6 billion). Owlstone is aiming to save 10,000 lives and save the NHS 245 million pounds a year with early detection of the disease using their technology.
Published by Medicaldaily.com



























