Master Regulator of Blood Stem Cells Discovered
Scientists have found that the absence of a type of gene can change the fate of blood stem cells, either becoming blood tissue cells or becoming heart muscle cells. This could lead to a new source of heart muscle cells (cardiomyocytes) that can be used to repair a damaged heart.
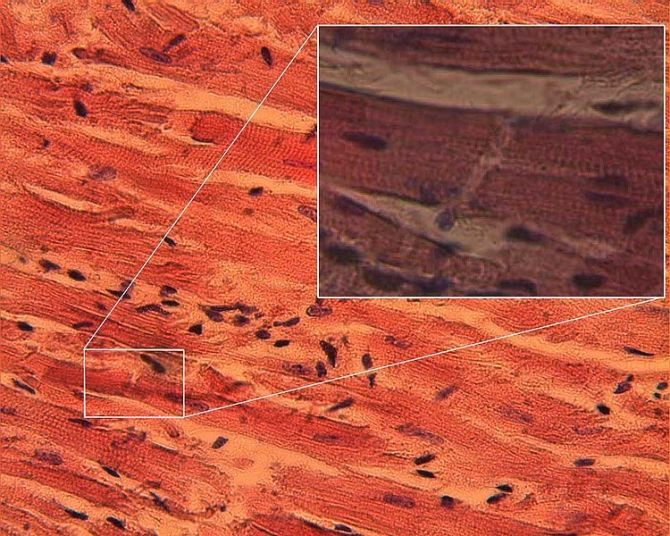
Blood stem cells give rise to all cell types that make blood tissue. New research suggests that whether a cell becomes blood tissue or a heart muscle cell depends on the presence or absence of a single transcription factor, Scl.
"Scl has a known role as a master regulator of blood development, and when we removed it from the equation, no blood cells were made. That the removal of Scl resulted in fully functional cardiomyocytes in blood-forming tissues was unprecedented," said Ben Van Handel, a University of California Los Angeles postdoctoral fellow and one of the authors of the study.
Researchers in the field of regenerative medicine have been looking at new ways to develop beating heart muscle cells since many years now. Recently, Medical Daily reported how skin cells can be reprogrammed to make heart muscle cells and the creation of an artificial jellyfish, made of rat muscle cells and silicone that can mimic human heart muscle.
"This study opens new ways to think about what could be a potential source of cardiac stem cells. We now have a better understanding of how cardiac progenitor cells can be made and regulated, and this may one day lead us to a way to treat heart attacks by creating new heart muscle cells to replace those that were damaged," said Dr. Hanna Mikkola, senior author of the study in a news release.
The research team used microarray technology to determine which genes were influencing the stem cells to create other kinds of cells. They found that in the absence of Scl, the genes that make heart muscle cells were activated.
"To make sure we had not switched the samples between blood-forming tissues and the heart, we ran the experiments again and repeatedly got the same results. It turns out Scl acts as a conductor in the orchestra, telling the other genes in the endothelium who should be playing and who shouldn't be playing," said Amelie Montel-Hagen, a postdoctoral fellow at UCLA and a co-author of the study.
The research team isolated the stem cells from yolk-sac of the embryos that lacked Scl. These cells became beating heart muscle cells in just 4 hours. They then tried to find if the stem cells' plasticity extended to other tissues like bone or kidney. They found that blood vessel cells could only change to heart muscle cells when Scl was absent and not to other related organs.
The study was published in the journal Cell.



























