Medical Ethics In America: Why Are More Doctors Disciplined For Bad Behavior In Some States Compared To Others?

Behind the lab coat, degrees, and stethoscope, doctors are ordinary people who are capable of mistakes and misbehavior. Where they differ from other professionals, though, is that their mistakes can end in death.
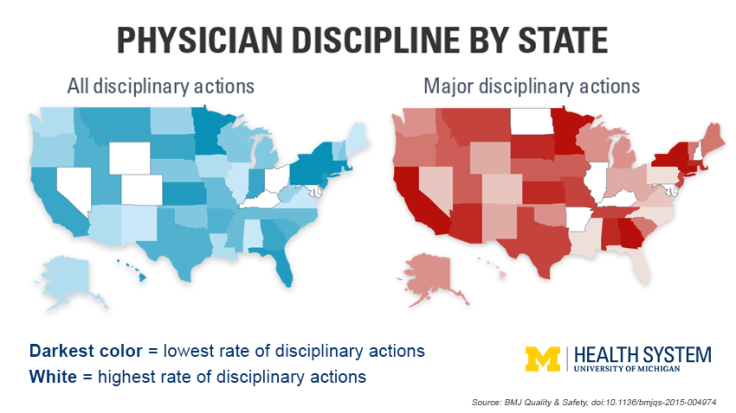
Researchers from the University of Michigan Medical School have found that the number of doctors who are either disciplined or required to pay out a malpractice claim is four times higher in certain states than it is in others. They say the problem isn’t cavalier doctors running around behaving poorly. Rather it’s the lack of standardized disciplinary regulations that monitor physician behavior nationwide.
"We don't know what the 'right' rate of physician disciplinary action is, but no state should want to be in the extremes," said senior author Dr. John A. Harris, in a statement. "Patients assume oversight of doctors is well-regulated in all states, that all doctors are held to the same ethical standards and disciplined appropriately when needed. But there's no central governing body, and there's significant variation."
Harris and his colleague, Dr. Elena Byhoff, gathered data on physician misbehavior between 2010 and 2014 in all 50 states and the District of Columbia using the U.S. Department of Health and Human Services' National Practitioner Data Bank. The research team focused on information regarding activities that required state medical boards to take action, including substance abuse, sexual misconduct, improper prescription writing, fraud, and negligence. They looked at specific penalties, including minor fines and the monitoring, revoking, or suspending of a doctor’s medical license.
Researchers used data on how much doctors paid in response to malpractice claims to represent what poor behavior among physicians lead to in each state. Although patients can’t access the data bank, hospitals, clinics, insurers, and medical boards use it to decide which doctors they use or hire. The team used all of the information they dug up to create yearly rates of all disciplinary actions per 1,000 doctors in each state.
"In one state the punishment for a particular violation could be a fine, while in another state you could lose your license for doing the same thing," said Byhoff. "It has implications for the ability of physicians to move from state to state."
Overall, there are 3.75 disciplinary actions — including 1.15 that were considered serious — each year for every 1,000 physicians in the U.S. Disparities begin to emerge from the data at the state level. Delaware scored highest with 7.93 actions per 1,000 physicians, 2.71 of which are major infractions. Massachusetts, on the other hand, had the lowest of all actions at 2.13 while New York had the lowest rate of major infractions at 0.64.
While the U.S. uses state-appointed medical boards to act as self-governing bodies that hand down punishments, most countries have adopted a nationwide system that oversees and punishes doctors who misbehave.
"Ultimately, don't we want all doctors operating in the same ethical way, and being disciplined appropriately if they fail to do so?" Harris added.
One of the most high-profile cases of physician misbehavior in America involved a New York-based obstetrician by the name of Dr. Allan Zarkin. After undergoing a Cesarean section done by Zarkin, Dr. Liana Gedz realized the initials “AZ” had been carved into her abdomen. Zarkin would eventually admit to being so proud of the successful operation that he decided to leave his mark, literally. For treating his patient “like a branded animal,” Zarkin received five years of probation and he was barred from applying for a medical license for five years.
This case and the precedent it set continues to reverberate in the current discussion of medical ethics. Zarkin eventually paid $1.75 million to settle a lawsuit with Gedz, but the slap on the wrist he received in terms of jail time concerned many. Especially considering the punishment someone without a medical degree would expect for slicing someone with a scalpel.
A more recent case involved Dr. Roger Ian Hardy, who was accused of molesting anesthetized female patients over a period of at least 10 years. What makes Hardy’s situation all that more terrifying is that the first complaint brought against him was in 2004. Nevertheless, he continued to work as a reproductive endocrinologist up until January 2014, when he resigned his medical license after a set of new allegations that were brought to the Massachusetts Board of Registration in Medicine. He maintains his innocence.
The U.S. has a national standard for the way doctors should behave thanks to the American Medical Association’s Code of Medical Ethics. Now, the University of Michigan research team suggests, we need a countrywide system for enforcing it.
Source: Byhoff E, Harris J. Variations by state in physician disciplinary actions by US medical licensure boards. BMJ Quality and Safety. 2016.



























