Misconception of a Top Antibiotic Drug Debunked and Made Simpler
A general misconception about how a frequently prescribed drug works to fight off infection has been debunked and revealed to be simpler than researchers had previously thought.
Researchers at the University of Illinois said in a released statement on Monday that the study findings could lead to the development and discovery of more novel and better treatments against systemic fungal infections that affect a wide range of patients including the elderly, chemotherapy or dialysis patients, and those with HIV or other immune disorders.
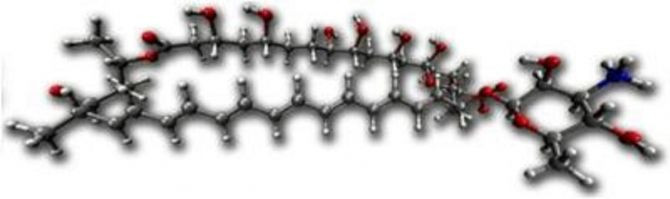
The scientists discovered that amphotericin, a top antibiotic for treating fungal infections despite its toxicity, works by binding to a lipid molecule that is essential to yeast’s physiology.
Experts have previously thought that amphotericin created ion channels that were capable in permeating cell membranes in order to cell infections, and possibly as well as the patient’s cell, and while the efficacy of the antibiotic was clear, researchers were unsure of the reasons for its “remarkable” infection-fighting ability.
"When I was in my medical rotations, we called it 'ampho-terrible,' because it's an awful medicine for patients," said study-author Martin Burke and chemistry professor at Illinois University in a statement.
"But its capacity to form ion channels is fascinating. So my group asked, could we make it a better drug by making a derivative that's less toxic but still powerful? And what could it teach us about avoiding resistance in clinical medicine and possibly even replacing missing ion channels with small molecules? All of this depends upon understanding how it works, but up until now, it's been very enigmatic," Burke said.
Researchers said that amphotericin binds to a lipid molecule called ergosterol which is prevalent in fungus and yeast cells to kill a cell, and that the drug doesn’t need to create ion channels at all.
Burke and his team produced a derivative of the antibiotic using molecule synthesis that could bind ergosterol but were unable to form ion channels and tested it against the original amphotericin, and found that the ergosteral-binding, non-channel-forming derivative was almost as potent as natural amphotericin were just as effective against two yeast cell lines, one of which is highly pathogenic in humans.
"The results are all consistent with the same conclusion: In contrast to half a century of prior study and the textbook-classic model, amphotericin kills yeast by simply binding ergosterol," Burke said. "The beauty is, because we now know this is the key mechanism, we can focus squarely on that goal. Now we can start to think about drug discovery programs targeting lipid binding."
Researchers are now focused on making a derivative that will bind to ergosteral in yeast cells and not to cholesterol cells, to see if it is possible to kill an infection without harming a patent. They also hopw to find other derivatives that would target lipids in fungi, bacteria and other microbes and aim to create a therapeutic strategy that would defy resistance.
"Now we have a road map to take ampho-terrible and turn it into ampho-terrific," Burke concluded.
The study findings are published in the journal Proceedings of the National Academy of Sciences.



























