Missed Connections: Spinal Surgery Software Helps Doctors Operate On Correct Vertebra
It isn’t unheard of for surgeons to write in big black permanent marker “THIS LEG” before operating on a patient — a small cost of pride compared to the full subtraction of a healthy limb. Now, scientists from Johns Hopkins University are trying to solve a similar, albeit more complex, breakdown in procedure: wrong-level spinal surgery.
The nature of spinal surgeries is such that even the most technically proficient radiologists can mistake one vertebra for those on either side of it. In a study published in Spine, researchers describe their new imaging software, LevelCheck, which helps surgeons supplement their existing level-counting strategies and avoid adding to the already underreported problem of wrong-level surgeries.
“It’s a looking problem,” Dr. Jeffrey Siewerdsen, lead author of the study and professor of biomedical engineering at JHU, told Medical Daily. “The vertebrae is so similar, just one on top of another. You count your way up, and there’s the potential for human error along the way.”
Current methods are frustrating at best and catastrophic at worst. If the surgeon is going in to do a spinal reconstruction — a relatively simple procedure, as far as spinal surgeries go — the worst he or she might do is extend the implant. “Maybe we meant for the construct of implants to span T10 to T11” — the 10th and 11th thoracic vertebrae — “and we see that we’re actually operating on T11 and T12,” Siewerdsen said, “so we say ‘OK, we’ll just extend the construct more than we originally intended.’ And the effect on the patient is probably very minor.”
But some cases, like those hoping to remove tumors, are more involved. Missing the target tissue could mean bringing a patient back in for surgery a second time. Or perhaps the stabilizing implants miss the weak points in the spine, so the patient doesn’t receive any additional benefit to the problem area. Getting hard data on these cases is tricky, Siewerdsen says, because it’s all self-reported, and many surgeons are reluctant to divulge mistakes. The best science can do in the future is simply to prevent them from happening.
LevelCheck tries to accomplish that goal. Siewerdsen and his colleagues worked on the technology based on pre- and intraoperative images of 20 patients. Tinkering with the image alignment, they found through 10,000 surgery simulations that the least amount of time the software needed to reach complete accuracy was 26 seconds.
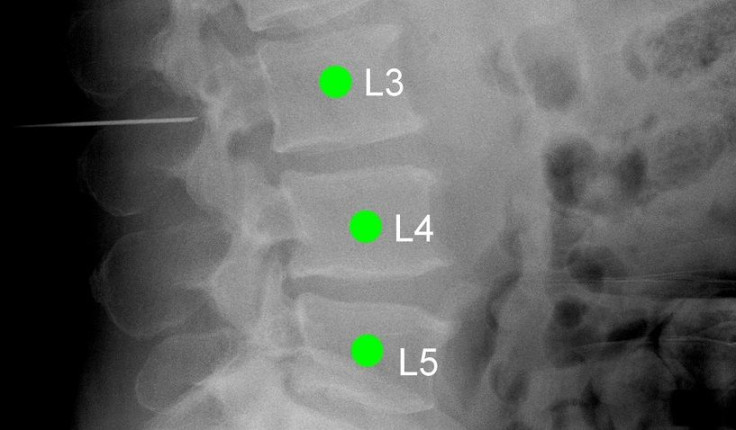
Here’s how it works: First, the patient undergoes a CT or MRI scan before the operation, so the doctor can visualize where the problem lies. Then the 3D scan, replete with the surgeon’s notes, gets fed through a simple computer program that aligns the image with a 2D x-ray taken in the operating room. A green marker pinpoints the correct vertebrae and assigns a label that the surgeon can use as a reference all throughout surgery.
Siewerdsen says the algorithm behind LevelCheck can be easily applied to target other areas of the body. “There’s actually nothing magic about this algorithm for the spine,” he said. “The way it operates is just to register any information at all that is labeled in the patient’s pre-operative image” on the x-ray print-out, called a radiograph. In theory, the technology could also help brain surgeons target areas in the brain for tumor removal, assist pelvic reconstruction, or repair tissues in the extremities.
The team hopes to further develop LevelCheck to where the technology becomes a mainstay in surgeons’ normal procedure, alongside normal CT scans and x-rays. They’re currently testing it out on a larger sample of 200 patients inside the operating room in real-time, and checking how well it can maintain accuracy and safety. In the meantime, Siewerdsen says, clinical trials suggest a more basic, immediate benefit.
“It actually just helps [surgeons] go a little bit faster with a little less stress.”
Source: Lo S, Otake Y, Puvanesarajah V, et al. Automatic Localization of Target Vertebrae in Spine Surgery: Clinical Evaluation of the LevelCheck Registration Algorithm. Spine. 2015.



























