MRSA Staph Infection Rates Fall By 50% In Hospital Settings Over 7-Year Period
The superbug known as MRSA (methicillin-resistant Staphylococcus aureus) has risen in popularity despite falling in prominence, according the latest report from the Centers for Disease Control and Prevention (CDC). MRSA staph infection rates have fallen in the last decade by more than 50 percent in hospital settings — one of the most common locations for the disease’s infection.
The greater prevalence of MRSA infections in hospitals and other healthcare facilities stems largely from improper hand washing procedures among facility employees as they move from patient to patient. While the CDC’s latest study cannot determine the cause of MRSA’s seven-year decline, between 2005-2011, researchers point to the improvement in these sanitation procedures as marking antibiotics’ greater success in staving off resistance.
"The good news is… the most serious kind of infection that lands people in hospitals and kills people is going down in the U.S.," Dr. Raymund Dantes, who led the study, said.
Dantes and his colleagues found 80,500 cases of MRSA infections in the United States in 2011. In 2005, that figure was up at 111,300. Rates among patients infected outside the hospital remained unchanged over the study period; however, the rates of hospital-acquired infection fell from about 9.7 infections per 100,000 people to about 4.5 per 100,000 people, Reuters reports. The team found infection rates among people who contracted the disease at home, after having just stayed in a hospital setting, fell 28 percent — from 21 infections per 100,000 people to about 15 infections per 100,000 people.
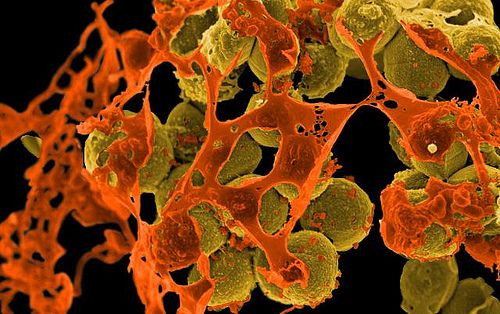
Staph infections stand out among other infections due to their deadliness once inside the bloodstream. Staphylococcus aureus bacterium lives on the skin of close to a third of the U.S. population without consequence; if an open cut or scrape lets the bacteria in, the dangers are far more present. MRSA is unique because it is resistant to antibiotic treatment with methicillin, one of the several types of penicillin. There is also a methicillin-sensitive strain of the infection, called MSSA.
“Although methicillin-resistant S. aureus (MRSA) strains are not necessarily more virulent than methicillin-sensitive S. aureus strains, some MRSA strains contain factors or genetic backgrounds that may enhance their virulence or may enable them to cause particular clinical syndromes,” one 2007 study on MRSA pathogenesis states.
People who are infected with the bacteria typically see red bumps appear on the skin, which eventually turn into larger sores. Within the body, the infection can attack bones, organs, and the bloodstream itself, making MRSA particularly lethal.
Despite hospital settings seeing declines, similar community-based settings saw no change. Controlling these areas now sits at the forefront of the CDC’s challenges, Dantes said.
"What's interesting about our study, we didn't see a big change … in the number of community-associated infections. So we haven't made as much progress getting those down," he said. "Certainly there is more research that needs to be done to understand community-associated invasive MRSA infections. So that's an area we're looking into more."
Dantes conceded that fully understanding how MRSA spreads outside of hospitals is tricky. As a general rule, he advises people to make active, and proactive, efforts to ensure that they maintain sanitary conditions as much as possible, which includes washing their hands on a regular basis.
People at higher risk for MRSA infections, such as those on kidney dialysis and people with diabetes, should take particular note of their hand-washing habits, according to Dr. Ghinwa Dumyati, an infectious disease physician at the University of Rochester Medical Center who worked on the CDC report.
"We're very optimistic,” she said, as “there are now more and more ways to prevent the transmission.”
Source: Dantes R, Mu Y, Belflower R. National Burden of Invasive Methicillin-Resistant Staphylococcus aureus Infections, United States, 2011. JAMA. 2013.
Published by Medicaldaily.com



























