Mystery Of Middle East Respiratory Syndrome Still Beguiles Researchers
In investigating Middle East Respiratory Syndrome Coronavirus (MERS), epidemiologists say a preponderance of infections among male members of a family in Saudi Arabia remains mysterious.
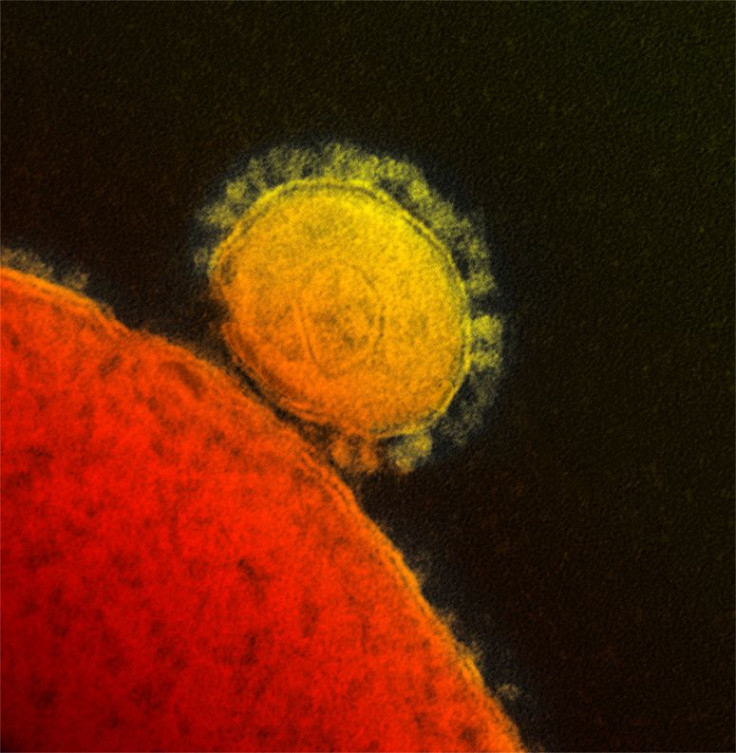
The kingdom first reported the new virus to the World Health Organization last September after a businessman died from acute respiratory and renal failure, with a total of 49 cases including 26 deaths by the end of May. The first of its kind known to infect humans, the virus belongs to the coronaviridae family, with a reputation for genomic plasticity and an ability to cause a range of infections in mammalian and avian species.
In November, the virus attacked an extended family living in Riyadh, with three confirmed cases and one suspected among scores of others in the family and general vicinity who went uninfected. The cluster attack began when a 70-year-old man fell sick in early October with fever, urinary retention, flank pain, diarrhea, renal colic, and urinary tract infection, admitted to the hospital days later with heart failure. In late October, he died in the hospital after suffering cardiogenic and septic shock. Five days later, the man's eldest son, 31 years of age, fell sick and was admitted to the hospital and later discharged after improvement of symptoms - but later returned with acute hypoxemia, dying two days later.
In a familial chain reaction, that man's own son, the 16-year-old grandson of the first patient, began wheezing just the next day, with fever, malaise, sore throat, and a cough. He stopped eating and was admitted to the hospital several days later with a high temperature, diarrhea, abdominal pain, myalgia, headache, and a worsening cough. However, blood tests returned normal liver and renal functioning with routine serum electrolytes, and his condition improved as he was treated with oral antibiotics.
However, the boy's uncle, the son of the first patient, had fallen sick the day after the boy began coughing and wheezing, and was later taken to the hospital with an acute onset of fever, rigors, and night sweats. He began coughing up blood and phlegm and was treated for coalescing airspace densities in his chest, in addition to leukopenia, and was soon breathing on his own with good vital signs and normal functioning of lung and renal gland. He was discharged from the hospital days later.
In the epidemiological mystery, many family members and a total of 124 health care workers came into contact with the first patient but were not sickened. Intriguingly, none of the women in the family reported a major respiratory illness from September to January, though they had all come into repeated contact with male family members infected with the virus prior to hospitalization. In addition, nine children under the age of 14 came into contact with the infected family members prior to their hospitalization, but none became sick.
An international team of epidemiologists published a report on Wednesday in the New England Journal of Medicine, reporting on "known unknowns" regarding the new disease.
"This report suggests that transmission of MERS occurred among family members but indicates that the risk of MERS infection among close contacts of patients is low, although infection risk is increased in patients with immunosuppression or coexisting illnesses," they wrote. "Although current data indicate that MERS does not appear to be as readily transmissible among humans, as was observed with the SARS epidemic in 2003, continued risk assessment, surveillance, and vigilance by all countries are required."
The researchers said countries around the world should remain vigilant about disease surveillance with regard to travelers who've returned home from the Middle East, for as long as 10 days.
Source: Memish ZA, Zumia AI, Al-Hakeem RF, Al-Rabeeah AA, Stephens GM. Family Cluster of Middle East RespiratorySyndrome Coronavirus Infections. New England Journal of Medicine. 2013.
Published by Medicaldaily.com



























