New Antidepressant May Bring Relief To Sufferers Of Major Depression In Just 5 Days

A new type of seroterotonergic antidepressant may improve treatment of major depression, by evincing a speedier response than existing serotonin agonists.
With promising results in the Petri dish and mouse model, drugs targeting a specific kind of serotonin receptor in the brain may offer a safer alternative to ketamine, sometimes used off-label to treat the most aggravated and drug-resistant cases of the disorder.
Scientists believe selective serotonin reuptake inhibitors, or SSRIs, increase levels of the neurotransmitter serotonin by preventing its reuptake into the presynaptic cell and thus leaving more available to bind with the postsynaptic receptor, an occurrence believed to affect mood and appetite, among other effects. In this class of antidepressants are the popular drugs, sertraline, sold generically and under the brand name Zoloft, and fluoextine, better known as Prozac.
Major depression affects one in 10 Americans and is the leading cause of disability around the world, with medicine limited today to current SSRIs, tricyclics, and monoamine oxidase inhibitors — drugs that either don’t work or take weeks to show any benefit. Typically, only 30 to 40 percent of patients respond to initial treatment with such antidepressants, with an average onset of response some two to four weeks after that first visit to the pharmacy.
"One of the biggest problems in the treatment of depression today is a delay in onset of therapeutic effects,” Stephanie Dulawa told reporters. “There has been a great need to discover faster-acting drugs.”
Although ketamine induces an antidepressant effect within hours, similar to the effects of the drug scopolamine, serious side effects exist for both, researchers say. At least one doctor in the United States, Demitri Papolos, founder of the Juvenile Bipolar Research Foundation, prescribes the drug off-label for children with drug-resistant cases of bipolar disorder — a move some see as controversial given lack of approval by the U.S. Food and Drug Administration for the use.
In a study published Tuesday, graduate student Mark Opal and his co-investigators at the University of Chicago cite recent work in rodent models suggesting ketamine’s efficacy in bringing rapid relief to sufferers of major depression, via a mechanism leading to rapid synaptic spine formation on specific dendrites within the brain’s prefrontal cortex.
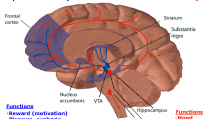
In similar fashion, the investigators sought to discover whether targeting a specific serotonin receptor, 2C (5-HT2C), would provide the same rapid effect. Interestingly, the serotonin receptor antagonists were mediated by dopaminergic signaling, which Opal called a “purely novel finding.” After five days of treatment, the drug began to work.
"We observed fast-acting therapeutic effects in multiple behavioral tasks [in depressed mice] after we administered compounds that selectively block serotonin 2C receptors," Opal said. "We began our measurements at five days, but we think there's a possibility it could be effective even sooner than that."
Stephanie Dulawa, an associate professor of psychiatry and behavioral neuroscience who led the study, said although some current antidepressants already affect those serotonin 2C receptors, they are not “selective,” and would thus bind with other receptors in the brain.
The researchers said they’re now investigating suitable compounds to target those receptors in clinical trials, given the method’s promise for delivering a safe and effective treatment for the worst of the worst in major depression.
Source: Opal MD, Klenotich S, Morais M, et al. Serotonin 2C Receptor Antagonists Induce Fast-Onset Antidepressant Effects. Molecular Psychiatry. 2013.
Published by Medicaldaily.com



























