New Blood Test Can Distinguish Between Viral And Bacterial Infections, May Curb Unnecessary Use Of Antibiotics
Both bacteria and viruses can ruin our day, our week, or even our life. People go to the doctor for unidentified ailments resulting in common symptoms like coughing, sneezing, and sore throats, sometimes only to be prescribed a drug that won’t help them at all. This is often the case when viruses are mistaken for bacterial infections, and patients are given antibiotics to consume even when they don’t really need them. This, in addition to the feeding of antibiotics to livestock, has contributed to the rise of antibiotic-resistant bacteria—a danger researchers predict will cause more deaths than cancer within a few decades.
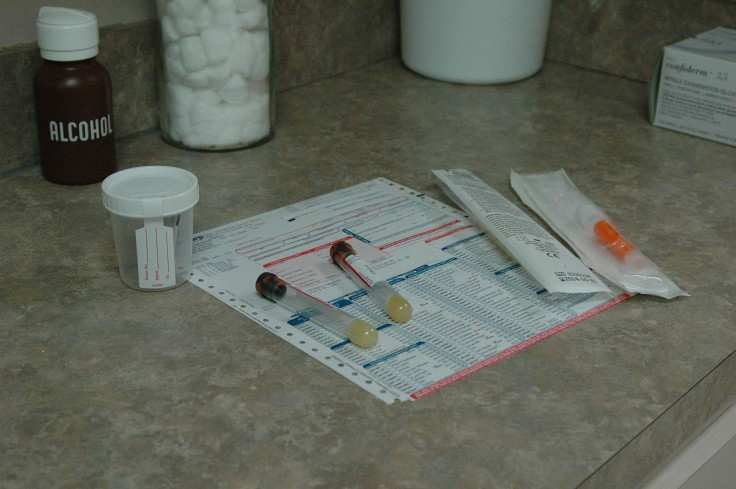
Aware of this ever-growing problem, researchers at Duke Health are working to fine-tune a blood test capable of determining whether a respiratory illness is caused by a virus or bacteria. Experts in infectious disease and genomics at Duke developed something they call gene signatures — patterns that indicate if a patient’s genes are turned on an off — that indicate if someone is fighting off a viral or bacterial infection. The results can be derived from just a bit of blood.
The signatures were tested in ab observational study and found to be more than 87 percent accurate when it came to classifying hundreds of patients with flu viruses, several strep bacteria, rhinovirus, and other common infections. They were also capable of detecting when there was no infection present. These findings represent a step forward in the fighr for a rapid blood test that could be used in clinics to guide appropriate antibiotic distribution.
“A respiratory infection is one of the most common reasons people come to the doctor,” said Dr. Ephraim Tsalik, lead author of the study and assistant professor of medicine at Duke, in a press release. “We use a lot of information to make a diagnosis, but there’s not an efficient or highly accurate way to determine whether the infection is bacterial or viral. About three-fourths of patients end up on antibiotics to treat a bacterial infection despite the fact that the majority have viral infections. There are risks to excess antibiotic use, both to the patient and to public health.”
A more precise manner of distributing antibiotics would not only reduce risks associated with unnecessary antibiotic use, but also help with the treatment of viruses, according to study senior author Dr. Geoffrey S. Ginsburg, director of Duke’s Center for Applied Genomics & Precision Medicine.
“Right now, we can give patients Tamiflu to help the recover from an influenza infection, but for most viral infections, the treatment is fluids and rest until it resolves,” Ginsburg said. “In the next five to 10 years, we will likely see new antiviral medications for common bugs like respiratory syncytial virus (RSV) and even rhinovirus, (the predominant cause of the common cold), and guiding treatment choices will be even more important.”
Ginsburg and his colleagues at Duke have been studying gene signatures in respiratory infections for almost ten years, but only recent advancements in technology have allowed the analyzation of a person’s genetic makeup, 25,000 genes at a time. This is the first study to distinguish between non-infectious illnesses and viral from bacterial infections at the molecular level. Though advancements have been great, it still takes about 10 hours to measure a gene profile from a patient’s blood. Researchers hope to create a one-hour test.
“The ideal scenario, should this test ultimately be approved for broad use, is you would go to the doctor’s office and receive your results by the time you meet with your provider,’ said senior author Dr. Christopher W. Woods, a professor of medicine and associate director at Duke’s genomics center. “We are working to develop a test that could be run in most clinical labs on existing equipment. We believe this could have a real impact on the appropriate use of antibiotics and guide the use of antiviral treatments in the future.”
Source: Tsalik E, G Ginsburg, Woods C, Henao R, Nichols M, Burke T, et al. Under the weather? A blood test can tell if antibiotics are needed. Science Translational Medicine. 2016.
Published by Medicaldaily.com



























