New 'Easy And Safe' Stem Cell Production Method Uses Novel Chemicals, Eliminating Risk Of Cancers And Mutations
First, there were stem cells — the progenitors of human life, blank slates that could become any cell in the body. Then, scientists found stem cells all over the human body, with specific functions: ones in the gut, the bone marrow, and even at the base of the hair follicle. More recently, the 2012 Nobel Prize was awarded to John Gurdon and Shinya Yamanaka for their technique of transforming any adult cell back into a stem cell by adding genes to the cell. This would reprogram regular cells into stem cells called induced pluripotent stem cells (iPS cells). Now, researchers in China have taken the process a step further and made the technique faster, easier, and safer by trading extra genes for the chemical treatment of cells in what they are calling CiPSCs, or chemically-induced pluripotent stem cells.
What They Did
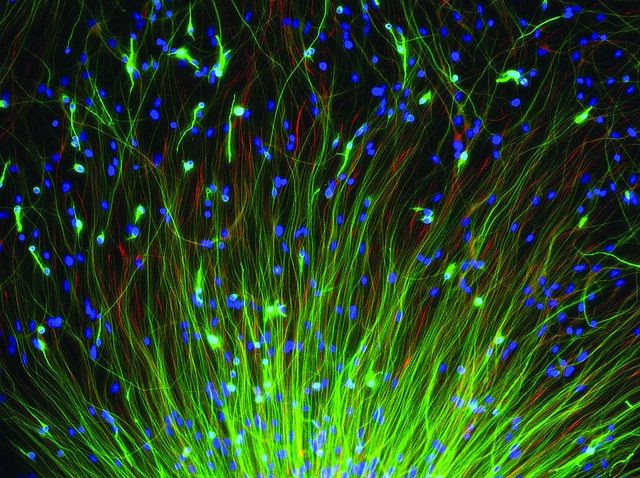
The standard technique previously used to turn adult cells into induced stem cells required adding in genes, a step that could lead the cells to gain mutations and even become cancerous. This would severely limit their ability to help patients and doctors to regrow organs and help heal wounds. To try to make stem cells from normal adult cells, which have already differentiated to become a specific cell type, researchers at Peking University in Beijing screened more than 10,000 small molecule pharmaceutical compounds and found seven that would turn adult cells from mice into stem cells, through a process of de-differentiation.
The rate at which the researchers were able to convert the adult cells into stem cells was small — 0.2 percent. But this is comparable to the rate that is used when scientists have inserted genes to do the same job. The advantage of using drugs to change adult cells into stem cells is that they can enter the cell easily, without activating the immune system — and it's cheap, fast, and standardized.
The scientists took the process a step further and induced the cells to turn into mouse embryos and implanted them into female mice. The mice were born and were healthy, proving that the cells could become any tissue type in the body, such as the brain, heart, and skin, under the right conditions. The amazing thing is that the mice born using this method were 100 percent viable and none died of diseases. The process worked so well that one of the cloned mice even gave birth to her own litter of babies, all of which are healthy.
What This Means For The Future
The team foresees using the technique on human cells in the future to treat patients with conditions that could be helped with regenerative medicine, including those with damaged hearts, spinal cord breakages, and severe skin burns.
The researchers also noticed something quite interesting, which ties in frogs and limb regeneration. Frogs are well-known to be able to regenerate a limb if it is severed, but mammals have lost this ability, even though we share a vast number of genes with the amphibians. The scientists in the current study saw that a gene expressed when a frog's limb regenerates, called Sall4, was also expressed early in the chemically-induced stem cells reprogramming process, unlike the traditional gene insertion process to make iPS cells.
This gives the researchers hope that someone who loses a limb or digit may be treated with a series of chemical compounds on their wound to regenerate their tissues, similarly to the process that occurs in frogs. But until research teams can determine what chemicals will work on human cells to reprogram them into stem cells, the research will remain in the laboratory.
Clinical trials using iPS cells, in which genes were added to adult cells to make them into stem cells, have been approved in Japan to treat a certain type of blindness by turning the cells into retinal cells. The trials should begin in September.



























