New Ovarian Cancer Screening, Based On Simple Blood Test, Shown Effective In US Study
A study of a new screening strategy for ovarian cancer has shown ‘value,’ according to U.S. researchers who have published their results on over 4,015 women in the journal Cancer. But an even larger study of the new screening strategy — 50,000 total participants — is now taking place in the United Kingdom. When researchers conclude this larger study within the next two years, the actual value of the screening should be certain, BBC reports. What’s most important, though, is the centerpiece of the new screening consists of a simple blood test.
Cancer Antigen
A woman’s ovaries are a pair of reproductive glands, each roughly the size of an almond, on either side of the uterus. The ovaries produce not only eggs but also the hormones estrogen, progesterone, and testosterone. Approximately 14,600 women die from ovarian cancer, the second most common type of gynecologic cancer, each year in the U.S.
A routine blood test can easily measure the amount of the protein CA 125 (cancer antigen 125) in the blood. Identified as a cancer antigen for some time, CA 125 has posed difficulties and, as a result, has never been considered accurate enough to use for screening of ovarian cancer. For instance, women in the earliest stages of ovarian cancer may register normal levels of CA 125, while common conditions sometimes boost levels of the antigen in the blood; normal menstruation as well as pregnancy can cause a spike in CA 125.
In order, then, to more accurately estimate the risk of ovarian cancer, researchers from the University of Texas decided to combine the results of a CA 125 blood test (along with a risk of ovarian cancer algorithm result, which is based in part on a woman’s health and age) with other assessments.
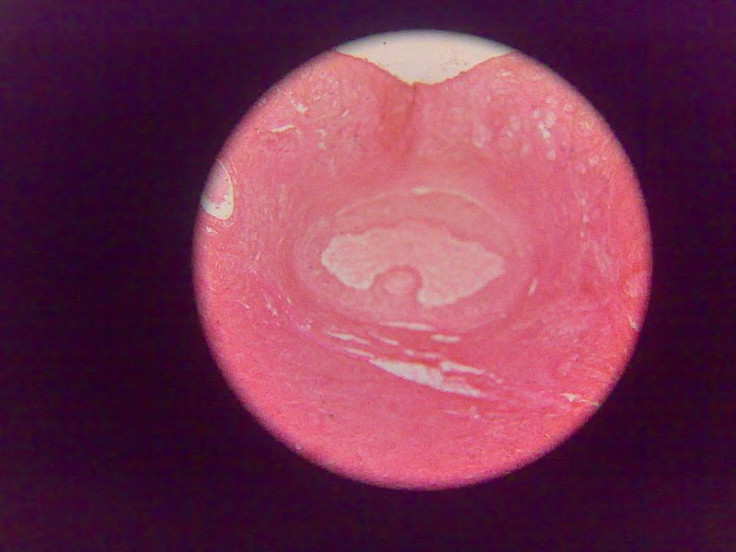
The study followed post-menopausal women for 11 years on average. After first testing for CA 125 level, the researchers then triaged the women into three separate groups. Low-score (low-risk) women were recommended for an annual CA125 test; intermediate-risk women were recommended to repeat the CA 125 test in three months; high-risk women were recommended for a transvaginal ultrasound (TVS) as well as referral to a gynecologic oncologist. As a result of the researchers' findings, a total of 10 women had surgery based on their ultrasound scan and all the cancers detected were at an early stage.
Although pleased with the insights derived from the American study, the researchers suggested that the UK study of 50,000 people would give definitive answers. "There are two big questions — do we see cancers at an earlier stage and do we decrease the number of deaths," Dr. Karen Lu, lead investigator, told the BBC.
Early Detection Key
Commenting on the results, Dr. Sarah Blagden, from the Ovarian Cancer Action Research Centre of Imperial College, London, noted that the small American study may not be definitive, but it indicates effective ovarian screening is possible. "In 2015 the results of the UKCTOCs study will become available and the results are eagerly anticipated, more so now that this American study has produced such encouraging results," Blagden told the BBC.
When ovarian cancer is found in its early stages, treatment is usually effective. Unfortunately, for many women, ovarian cancer goes undetected until it has spread within the pelvis and abdomen. At later stages, it is much more difficult to treat and often becomes fatal.
According to the Centers for Disease Control and Prevention, older women are at higher risk for ovarian cancer than younger women with about 90 percent of incidence in women older than 40 and the greatest number of cases occurring in women aged 60 or older. Each year, about 20,000 women get ovarian cancer in the U.S., where it is the fifth leading cause of cancer death, after lung and bronchus, breast, colorectal, and pancreatic cancers.
Source: Lu KH, Skates S, Hernandez MA, et al. A 2-stage ovarian cancer screening strategy using the Risk of Ovarian Cancer Algorithm (ROCA) identifies early-stage incident cancers and demonstrates high positive predictive value. Cancer. 2013.



























