No More Needles? Experimental Insulin Patch Could Someday Help People With Diabetes
People with diabetes, especially children, find daily insulin injections a hard lot to bear. But soon, this repeated painful experience may become a distant memory. Researchers at the University of North Carolina and North Carolina State have created a smart patch that can detect increases in blood sugar levels and secrete doses of insulin into the bloodstream whenever needed. So far tested only on mice, the patch — just a thin square no bigger than a penny — shows great promise for human patients.
"We eventually want to commercialize this," Dr. Zhen Gu, senior author of the study, told Medical Daily. "We are trying to do a large animal study, and, if we are successful, we will move to human clinical trials."
Vesicles
Diabetes affects more than 387 million people worldwide. The difficulty of this disease is not the insulin shots, the blood sugar checks, or the special diet — it’s all three of these things, combined and performed several times a day, every single day. Unfortunately, people with diabetes cannot take a vacation day from their illness. In the past, researchers have tried to create "closed-loop systems" composed of mechanical sensors and pumps that track blood sugar and automatically administer insulin, however, these awkward, overly bulky systems have satisfied no one, neither scientist nor patient.
Gu, a professor of biomedical engineering, decided to emulate the body's very own beta cells. These versatile cells not only function as factories and warehouses, making and storing insulin in tiny sacs called vesicles, they also work as sensors, detecting fluctuations in blood sugar levels and signaling the release of insulin into the bloodstream.
To begin, Gu and his lab team constructed an artificial vesicle using two natural materials. Hyaluronic acid is an ingredient found in many cosmetics, while 2-nitroimidazole, an organic compound, is used in diagnostics. Combining these two ingredients, the researchers created new molecules that naturally congregated together and assembled themselves into millions of bubble-like structures, each 100 times smaller than the width of a human hair.

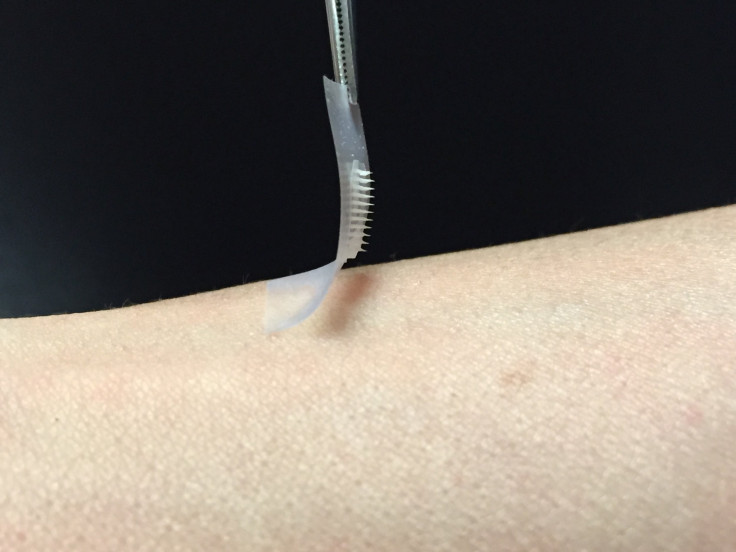
Next, the researchers injected insulin and enzymes (specifically designed to sense glucose) into each of their newly created vesicles or, in their words, "intelligent insulin nanoparticles." Then, Gu and his colleagues worked on the patient end of the equation. The research team worked to incorporate the sugar-sensing, insulin-releasing material into an array of micro-needles, which they created by using a different, more rigid form of the same material that went into the nanoparticles.
Finally, the science team arranged more than one hundred of these micro-needles on a thin silicon strip. Though it looks just like a doll’s house version of a bed of nails, this patch is painless when placed on the skin. Still the micro-needles are able to tap into the blood flow of capillaries just below the surface.
Tested on mice, the researchers found the smart patch worked to control blood sugar levels, while having the ability to maintain blood glucose for several hours. The patch works fast, is easy to use, and is made from nontoxic, biocompatible materials, Gu explained.
"I think the earliest it could be commercialized would be after two or three years," Gu told Medical Daily. If refined and approved for human use, this simple-seeming patch could potentially help millions of patients with type 1 and advanced type 2 diabetes worldwide.
“If we can get these patches to work in people, it will be a game changer,” Dr. John Bernard Buse, a co-author of the study and past president of the American Diabetes Association, stated in a press release.
Source: Yu J, Zhang Y, Ye Y, et al. Microneedle-array patches loaded with hypoxia-sensitive vesicles provide fast glucose-responsive insulin delivery. PNAS. 2015.
Published by Medicaldaily.com



























