Obamacare Compromise Creates Coverage Gap For One-Quarter Of Uninsured: Will States Offer More Funding?

A hodgepodge of compromises, the Affordable Care Act (ACA) creates a coverage gap for one-quarter of Americans lacking healthcare insurance in states opting out of the Medicaid expansion.
In forgoing a push for universal healthcare under a single-payer model, the original authors of the new federal healthcare law intended to allocate federal funds to provide Medicaid for people with incomes up to 138 percent of the federal poverty level. Yet, the U.S. Supreme Court’s historic ruling last year permitted to states to reject the Medicaid expansion, while also requiring every American to carry healthcare insurance under penalty of a “tax.”
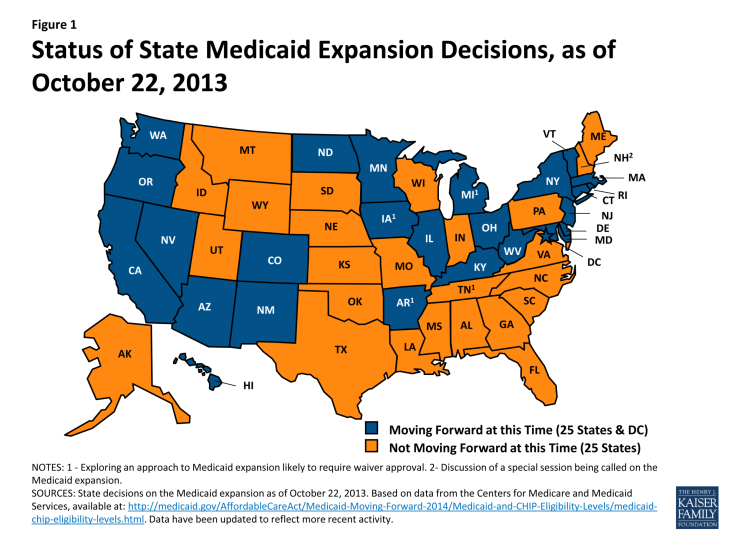
That controversial 5-4 ruling, with a surprise blessing from conservative Chief Justice John Roberts, left the country divided neatly in half, with the expansion or rejection of Medicaid expansion approximating the Red-Blue partisan lines. Presently, 21 states have declined to participate in the Medicaid expansion, funded mostly by the federal government, while four others are considering it.
Currently, 27 percent of uninsured U.S. residents fall into a newly formed coverage gap. In states opting out of the Medicaid expansion, these Americans do not qualify for traditional Medicaid because of income they do not belong to a specific group, such as adults with dependents. But they also make too little money to qualify for new federal subsidies available for people earning one to four times the federal poverty level.
Denise Rodriguez, an attorney in Los Angeles, told Government Health IT, “It is highly unlike that those people would be able to afford coverage [via the exchanges] without the subsidy and, as a result, they would remain uninsured.
Traditionally, Medicaid covered only a portion of America’s poor uninsured, such as families with children, the elderly, and the disabled. Last year, only 30 percent of the rest of the uninsured population received coverage from Medicaid, with most states choosing not to provide eligibility for the state-federal program, according to the Henry J. Kaiser Foundation. By contrast, Medicaid covered 70 percent of poor children.
Poor adults were more than twice as likely as others to go without insurance, at a national rate of 42 percent compared to 18 percent overall. By expanding Medicaid eligibility to every American at 138 percent of the poverty level, or roughly $27,000 for a household of three, many uninsured would gain coverage next year in the 25 participating states.
The preponderance of Americans falling into this new coverage gap live in Florida, Georgia, Texas, Alabama, Louisiana, and Mississippi. However, Texas and Alabama both set lower eligibility thresholds than other states opting out of Medicaid, with residents qualifying at 19 percent and 16 percent of the federal poverty level, respectively. Four other states — Alaska, Maine, Tennessee, and Wisconsin — cover parents with children at an income threshold up to the federal poverty level.
Among states opting out of Medicaid expansion, the median income eligibility is 49 percent of the federal poverty level, meaning a single mother working part-time at minimum wage would likely make too much income to qualify. Next year, that median rate will fall slightly to 47 percent of the federal poverty level.
A Commonwealth Fund study says that 40 percent of those falling into the coverage gap will not find any new affordable healthcare options next year.
Published by Medicaldaily.com



























