Once Monthly, After-Sex Birth Control Pill Can Be Developed; Getting Past Political Opponents Is The Problem
The United States currently defines pregnancy as implantation of a fertilized egg onto the uterus. By this definition, birth-control methods, which really only focus on preventing pregnancy pre-fertilization, could also be developed to prevent pregnancy post-fertilization. Such a method would be welcomed by women for various reasons, however, political opposition would surely call it abortion, the authors of a recent editorial say.
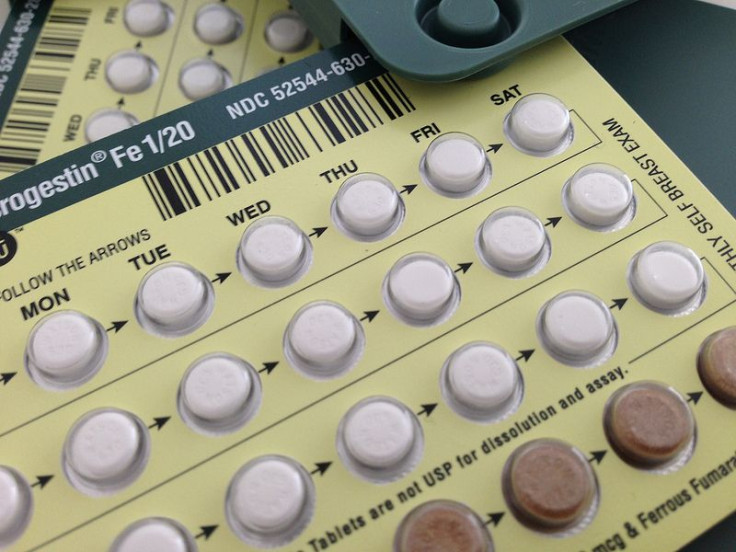
Perhaps the most alluring benefit of a post-fertilization contraceptive would be that it could only be used once a month, regardless of how many times a woman had sex, and even if they had just missed their period. For the roughly 25 to 35 percent of women who are sensitive to the hormones in birth control pills — usually experiencing emotional and sexual side effects — a once monthly pill could be the answer. Additionally, women who aren’t as sexually active wouldn’t have to take the pill almost daily just to be safe.
“Post-fertilization methods would eliminate the conceptual and logistical challenge of needing to obtain and initiate contraception before having sex, which can be daunting for both men and women,” the authors of a study, which was the subject of the editorial, wrote.
Getting the idea past political opposition would be the first hurdle, the authors wrote. That’s because many anti-abortion activists believe life begins at fertilization. “What these researchers are calling for is nothing less than the routine provision of an abortion pill for women,” Norman Wells, of England’s Family Education Trust, told the Daily Mail. “The licensing of this kind of drug would effectively introduce abortion on demand by the back door. To call a drug a contraceptive when it is designed and intended to be used after intercourse, and potentially after fertilization is a complete misnomer.”
However, the authors note that some contraceptive methods already in use, such as intrauterine devices, occasionally end pregnancy after fertilization, and before implantation. “We should openly acknowledge that some of the most effective standard contraceptives probably act, at least in part, after fertilization,” the authors wrote, according to LiveScience.
After political opponents, developers would need to look at which chemical compounds would be used in the drug. There are already “promising compounds and the pharmaceutical know-how to develop them,” but understanding how they would work in post-fertilization is still unclear.
“We need to stop extolling pre-fertilization contraception as a good thing, because it implies that something that works after fertilization is bad. We have to stop doing that,” Elizabeth Raymond, senior medical associate at Gynuity Health Projects in New York, said in the editorial. “[Post-fertilization] contraception doesn’t have to be acceptable to every woman. No method of contraception is acceptable to every woman now.”



























