Parkinson’s Drug, Benztropine, Reverses Multiple Sclerosis: New Progress For Regenerative Treatment
Although Parkinson’s disease and multiple sclerosis (MS) have little in common clinically, besides being paralyzing neurological disorders, a report in Nature reveals a drug for the former offers a new path for treatment of MS.
"We're excited about these results, and are now considering how to design an initial clinical trial," said chemist and senior author Dr. Luke Lairson of The Scripps Research Institute, who found that the Parkinson’s drug, benztropine (Cogentin), could repair a feature of MS that current drugs do not confront.
Mulitple sclerosis, which afflicts 2.3 million worldwide, is a disease with two sides.
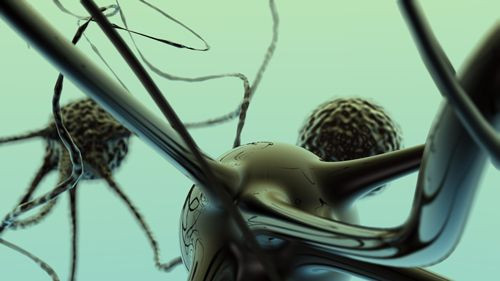
First, there is autoimmunity, where the body’s immune system attacks the brain’s myelin. Like asphalt on the roadways that connect individual neurons, myelin makes transporting messages between brain cells less bumpy and faster.
The other half of the disease involves special cells that can repair myelin, known as oligodendrocytes. For an unknown reason, these cells stop growing during MS and are especially absent during remission stages of the disease.
"Oligodendrocyte precursor cells (OPCs) are present during progressive phases of MS, but for unknown reasons don't mature into functional oligodendrocytes," Lairson continued.
Most prevailing remedies for MS target autoimmunity, but do little to promote oligodendrocytes, so Lairson and his colleagues performed a drug screen to search for compounds that would target this underserved realm of MS.
Their top hit — benztropine — reversed MS symptoms and virtually eliminated the disease’s ability to relapse in mouse models, according to the authors.
“In the mice it had profound efficacious effects," Scripps immunologist and senior author Dr. Brian Lawson told Nature News. “At the peak of disease, when the mice were most severe paralyzed, in just a number of days, you could almost not tell them from regular mice.
The drug, which is already approved by the Food and Drug Administration (FDA), worked by itself, but also when paired with existing immune-suppression therapies.
"Adding even a suboptimal level of benztropine effectively allowed us, for example, to cut the dose of fingolimod [Gilenya] by 90%—and achieve the same disease-modifying effect as a normal dose of fingolimod," Lawson continued. "In a clinical setting that dose-lowering could translate into a big reduction in fingolimod's potentially serious side effects."
Benztropine, however, is associated with its own set of dose-dependent side effects, and the authors caution against using it off-label before further tests demonstrate that it is safe for human MS patients. The Scripps team is setting up an initial clinical trial.
"We're also looking at some of the other, relatively unknown molecules that we identified in our initial screen, to see if any of those has better clinical potential than benztropine," Lairson concluded.
Source: Deshmukh VA, Tardif V, Lyssiotis CA, et al. A regenerative approach to the treatment of multiple sclerosis. Nature. 2013.



























