Patients With Atrial Fibrillation, Heart Failure May Not Benefit From Digoxin
It might come as a surprise, but many of the longest established medical treatments available in our doctor’s toolkit have little rigorous research to support their effectiveness and safety.
Before the era of regulated clinical trials that can take years to clear a new drug to be publically available, doctors more often than not relied on the anecdotal, trial-and-error, case reports of their respective fields to determine whether any particular treatment worked. That isn’t to say that these drugs and therapies don’t actually work, and work quite well (aspirin), so much as it is to say that there could be possible potholes that have remained hidden under the inertia of medical tradition. This past Monday, researchers in the European Heart Journal may have uncovered such a bump, finding that the heart drug staple Digoxin is associated with a 21 percent risk of early death among its users.
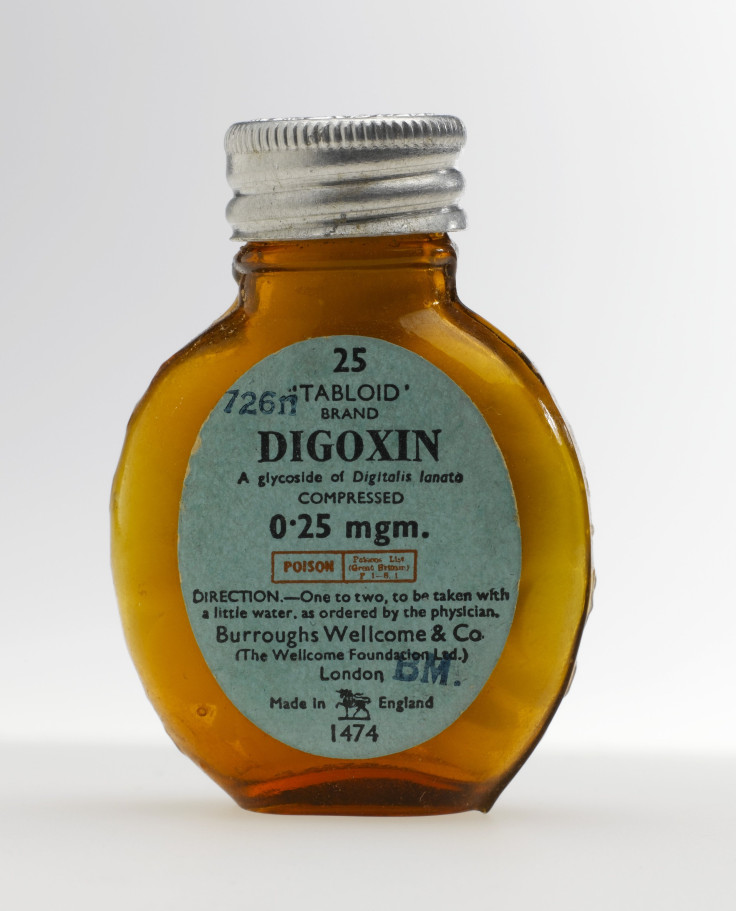
Originally derived from the foxglove plant, digoxin has been touted for more than 200 years as a medication that can decrease heart rate and increase blood pressure. These effects have enabled it to be useful for people suffering from atrial fibrillation (AF), an abnormal heart rhythm characterized by a rapid and irregular beat, and other related forms of heart failure. While similar, more toxic, compounds have dropped out of favor, digoxin has remained a stalwart of heart treatment, with the World Health Organization placing it on its list of essential medicines needed for a basic health system.
But as the authors of this current study explain, the evidence base for digoxin is scant, with only one randomized controlled study in existence, albeit one that did find digoxin reduced the rate of hospitalizations as a result of heart failure. What has been known for a while though is that digoxin is a fickle drug that doesn’t interact well with other heart medications and that needs to be given in precise monitored doses in order to prevent severe side effects. Its reputation preceding it, several studies have reported an increased rate of mortality with even careful digoxin use, and some doctors have even questioned whether it should be implanted at all anymore. With that in mind, the authors conducted an exhaustive review of studies involving digoxin, focusing primarily on its use with AF and congestive heart failure (CHF) patients.
Ultimately looking at 19 studies that contained data on over 300,000 patients, their conclusions were undoubtedly sobering. “Based on the analysis of all 19 trials, digoxin use was associated with an overall 21 percent increased relative risk of all-cause mortality compared with patients not receiving this medication,” the authors wrote. Breaking it further down, they found a 29 percent increased mortality risk among 235,047 AF patients, and a 14 percent increased risk among 91,379 CHF patients.
The authors, careful to note that these reviews are not the be-all, end-all of medical knowledge, nonetheless call for further studies of digoxin, and to change the current guidelines of its use in the meantime. “Until such proper randomized controlled trials are being completed, digoxin should be used with great caution (including monitoring plasma levels), particularly when administered for rate control in AF,” they wrote.
Luckily for those for rapidly fluttering hearts, while digoxin has remained popular, it’s no longer on the front lines of treatment, with more recent and better tested groups of drugs like beta blockers currently available for use.
It appears that time and a little more research will tell us if digoxin’s glory days are long behind it.
Source: Vamos M, Erath J, Hohnloser S. Digoxin-associated mortality: a systematic review and meta-analysis of the literature. European Heart Journal. 2015
Published by Medicaldaily.com



























