Placebo Effect: Depression Patients Who Respond Well To Fake Treatment Also Recover Faster When They're On The Real Thing

Our psyches have a huge impact on how we perceive things and even how we recover from illness; research has shown that positive thoughts can lead to a longer life, lower rates of depression and anxiety, and a more protected immune system and heart. This is perhaps why placebos — or a fake pill or drug that has no physical benefit, but makes someone believe they are healing — can have such a powerful effect on us.
A new study, published in JAMA Psychiatry, examined the power of the placebo in depression patients. The researchers, out of the University of Michigan Medical School, found that depressed patients who benefited psychologically from a placebo drug actually fared better when they took real antidepressants. In other words, people who are prepared to recover from depression — determined to overcome its dark hold — are more likely to benefit from depression drugs and treatments. Their brain chemistry changes while on the placebo, and thus it’s more likely to change when it’s on real drugs.
Enhancing Natural Resiliency
In previous research, the same team found that the mu-opioid system in the brain, its natural “painkiller” mechanism, was activated by placebos — and they wanted to understand this further.
In the latest study, they examined 35 participants with untreated major depression. The researchers reviewed the participants’ brain chemistry while they were given a placebo drug and told it was a new depression drug. For two weeks, the patients were on a placebo pill, then received a brain scan, as well as a placebo injection of salt water that they were told may have anti-depressant properties. Afterward, they were given a real anti-depressant.
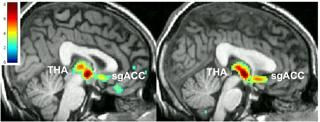
Patients who reported an improvement during the placebo experienced the most mu-opioid response in brain regions associated with emotion and depression; they were also more likely to see benefits with the real drugs. The researchers believe that certain people — perhaps due to a genetic predisposition — were more likely to be impacted by the placebo effect than others.
“These results suggest that some people are more responsive to the intention to treat their depression, and may do better if psychotherapies or cognitive therapies that enhance the clinician-patient relationship are incorporated into their care as well as antidepressant medications,” Dr. Jon-Kar Zubieta, an author of the study and chair of the Department of Psychiatry at the University of Utah, said in the press release. “We need to find out how to enhance the natural resiliency that some people appear to have.”
Researchers have attempted to harness the power of the placebo in treating depression and other illnesses for some time now. In 2014, UCLA released research that found that the placebo effect was closely tied to people’s expectations when using it. Patients who expected the pill to work saw more improvements in their health than people who didn’t.
“In short, if you think a pill is going to work, it probably will,” Andrew Leuchter, the author of the UCLA study and a professor of psychiatry at the UCLA Semel Institute for Neuroscience and Human Behavior, said in the press release.
Perhaps then, new research can focus on how we can boost natural resiliency in certain people rather than rely solely on proven anti-depressants. Everyone is different and will react uniquely to depression treatments, and perhaps the most effective pathways are those that empower a person’s own sense of recovery.
Source: Peciña M, Bohnert A, Sikora M, Avery E, Langenecker S, Mickey B. Association Between Placebo-Activated Neural Systems and Antidepressant Responses. JAMA Psychiatry. 2015.



























