Preteens Failing To Get HPV Vaccine, CDC Says: Is Health Of The Next Generation At Risk?
What virus infects nearly 80 percent of sexually active women before the age of 50?
Human papillomavirus, or HPV, is the most common sexually transmitted infection in the U.S. with approximately 79 million Americans currently infected, and about 14 million people newly infected each year. HPV is actually a group of more than 150 related viruses and more than 40 of these can be easily spread through direct skin-to-skin contact during sex. Though there are many strains of HPV, only about a dozen have been identified as causing cancer of the cervix, anus, penis, vagina, or mouth, according to Dr. Oz. Specifically, types 16 and 18 together are believed to be responsible for the majority of cancers associated with the virus and up to 70 percent of cervical cancers.
The good news? Two HPV vaccines are currently available in the U.S. What's more, the Affordable Care Act requires most private health insurance plans to cover the entire cost so parents do not have to add a co-pay or contribute to a deductible for the HPV vaccine.
The bad news? Not enough people are receiving an HPV vaccine, according to representatives from the Centers for Disease Control and Prevention (CDC) and the American Academy of Pediatrics, who held a joint press conference today to discuss why progress in the fight against HPV has stalled.
Inoculation
According to data from the 2012 National Immunization Survey-Teen (NIS-Teen) released by the CDC, HPV vaccination rates in girls aged 13-17 years not only failed to increase between 2011 and 2012, but also declined slightly in that time period.
Even worse, 84 percent of those girls who are unvaccinated for HPV had a healthcare visit where they received another vaccine (such as one aimed at meningitis or pertussis), yet they did not receive the HPV vaccine, reports the CDC. By way of comparison, in 2007, the percentage of unvaccinated girls who had a similar 'missed opportunity' for HPV vaccination amounted to only 20.8 percent. "Doctors need to step up their efforts by talking to parents about the importance of HPV vaccine just as they do other vaccines and ensure its given at every opportunity," said Tom Frieden, M.D., M.P.H., CDC Director.
The reason HPV vaccination is recommended for 11 and 12 year olds is that the vaccine works best when a boy or girl has time to develop an immune response before becoming sexually active with another person. HPV vaccines are given as a series of three shots over six months. Both of the vaccines — HPV2 (Cervarix, produced by GlaxoSmithKline Biologicals) and HPV4 (Gardasil, produced by Merck & Company, Inc.) — protect against the two most dangerous strains, types 16 and 18. HPV4, though, protects against an additional two strains, HPV types 6 and 11, which cause 90 percent of genital warts. Both vaccines are available for females. Only Gardasil is available for males.
The 2012 NIS-Teen asked parents who did not intend to vaccinate their daughters in the next 12 months (23 percent of respondents) the main reason why their daughters would remain unvaccinated.
The top five responses?
- vaccine not needed (19.1 percent)
- vaccine not recommended (14.2 percent)
- vaccine safety concerns (13.1 percent)
- lack of knowledge about the vaccine or the disease (12.6 percent)
- daughter is not sexually active (10.1 percent)
"Parents need reassurance that HPV vaccine is recommended at 11 or 12 because it should be given well in advance of any sexual activity," said Frieden. "We don't wait for exposure to occur before we vaccinate with any other routinely recommended vaccine."
Vaccine Safety
"HPV vaccine has been in use around the world for several years and has been very safe," the CDC states. The agency notes that the Vaccine Adverse Event Reporting System (VAERS) received a total of 21,194 adverse event reports occurring in females after receiving the Gardasil vaccine between June 2006 and March 2013. Of these reports, the overwhelming majority — 92.1 percent — were classified as nonserious adverse events, such as fainting, dizziness, nausea, headache, fever, and hives.
Among the 7.9 percent of Gardasil-related reports classified as serious, the most frequently reported symptoms were headache, nausea, vomiting, fatigue, dizziness, fainting, and generalized weakness.
Overall reporting of adverse events to VAERS is consistent with clinical trial data that was conducted before the vaccine was approved by the Food and Drug Administration (FDA). Although one observational study conducted after the vaccine was approved found an increased risk for fainting, no serious safety concerns have been identified in these large observational studies conducted after FDA approval.
Significantly, reporting of HPV vaccine-related events to VAERS peaked in 2008 and then decreased each year thereafter.
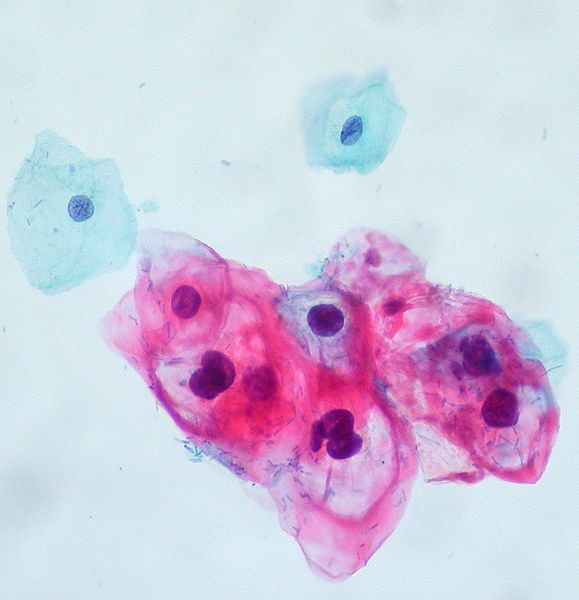
HPV Testing
Most gynecologists test their patients for HPV as a matter of routine. Women are tested by use of the Pap smear. In some cases or at those times when HPV has already been detected and needs to be monitored, the doctor will use a colposcopy and/or HPV DNA test. Although nearly all sexually active women will get at least one type of HPV at some point in their lives, half will clear the virus within eight months while a full 90 percent will clear the virus within two years. Whether or not the immune system completely 'clears' the virus in every case that it is said to have done so, however, is open to debate. Some believe that the body may develop antibodies that suppress HPV to the point that it may be undetectable on tests although the virus is still present. For this reason, it is wise to consider vaccination of children.
Final thought: although adequate tests exist for women, the FDA has not yet approved a test that can detect HPV in men with accuracy.
Source: Centers for Disease Control and Prevention. The Morbidity and Mortality Weekly Report. 2013.
Published by Medicaldaily.com



























