Psychotic Voices In Your Head Depend On Culture You’re From: Friendly In Ghana, Evil In America
How we hear hallucinatory “voices," either as the result of schizophrenia or some other undiagnosed condition, may depend largely on the culture in which we live, a new Stanford University study finds.
The new findings could lead to profound clinical changes in how people receive treatment for mental health disorders that trouble them — indeed, to deplete the disorders of their stigma and to reframe them as an ordinary part of life. In the U.S., in particular, where mental health services continue to lag behind the management of one’s physical health, offering a non-pharmaceutical outlet for schizophrenia could hold enormous potential.
“Our work found that people with serious psychotic disorder in different cultures have different voice-hearing experiences,” said lead author and Stanford anthropologist, Tanya Luhrmann, in a press release. “That suggests that the way people pay attention to their voices alters what they hear their voices say.”
Luhrmann and her colleagues conducted a total of 60 interviews, with 20 people each in the cities of San Mateo, Calif.; Accra, Ghana; and Chennai, India. Each subject was asked to describe the voices he or she heard, what the voices said, the tones in which they said it, and what each subject thought was causing the voices. "We asked people what they found most distressing about the voices, whether they had any positive experiences of voices, and whether the voice spoke about sex or God,” Luhrmann added.
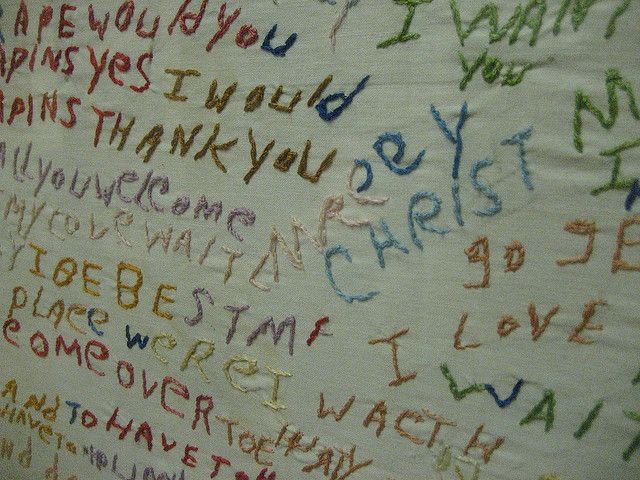
The differences were stark. Not one of the 20 Americans interviewed said the voices were pleasant or welcoming. Instead, they described them as violent, hateful. They cited the voices as evidence of a sick condition. One participant, in fact, described the voices as "like torturing people, to take their eye out with a fork, or cut someone's head and drink their blood, really nasty stuff." Meanwhile in Ghana and India, the stories played out very differently. More than half of the Chennai group said the voices were of family members, asking them to perform tasks. Half of the Accra subjects reported the voices as positive. Sixteen said they heard God.
Crossing Cultural Lines
Western ideas about schizophrenia bill it as a condition to be treated. Hearing voices is abnormal, and things that are abnormal need tiny white pills two times a day to balance them out. Outside the West, these ideas would be alien. Luhrmann points to each region’s varied sense of self. In India and Ghana, people conceived of themselves as one part of a much larger social machine. Entire groups had identity, not singular beings. In the West, of course, people are independent. We see ourselves as acting in isolation.
By and large, these conceptions influenced how people treated their disembodied visitors. In a country like India, where the people were more inclined to justify hallucinations as part of a natural social world, voices aren’t bad by default. They’re normal. Likewise in Ghana, external voices fit in nicely in the culture, where the Accra subjects reported high levels of religious observance.
"Actual people do not always follow social norms," the researchers conceded. "Nonetheless, the more independent emphasis of what we typically call the 'West' and the more interdependent emphasis of other societies has been demonstrated ethnographically and experimentally in many places."
For clinical applications, this translates into shifts in attitude. India and Ghana seem at ease with what we Americans would label a disease, mostly because they don’t call it a disease. They “explain away” the phenomenon, to borrow a term from psychology, as something already familiar to them. We, however, in a country where prescriptions are written at the drop of a hat, use medicalization as our default. Luhrmann and her colleagues say this is the wrong approach.
"More benign voices may contribute to more benign course and outcome," they wrote. Doctors should work toward forging positive relationships between patients and their voices. Rather than take an approach to therapy that automatically writes the experience off as disorder, they should first consider working with the voices, not against them. This tactic, while perhaps more time-dependent, requires the least amount of money or effort.
"Our hunch is that the way people think about thinking changes the way they pay attention to the unusual experiences associated with sleep and awareness,” Luhrmann said, “and that as a result, people will have different spiritual experiences, as well as different patterns of psychiatric experience.”
Source: Luhrmann T, Padmavati R, Tharoor H, Osei A. Differences in voice-hearing experiences of people with psychosis in the USA, India and Ghana: interview-based study. British Journal of Psychiatry. 2014.
Published by Medicaldaily.com



























