Self-Healing Hydrogel Offers Replacement To Invasive Surgical Implants For Drug Delivery
Even the innovations are innovating: A team of chemical engineers at MIT have developed a new self-healing hydrogel that is poised to replace current surgical implants used for drug delivery.
The findings have been published in a recent issue of Nature Communications. They show the success of a two-component system for getting patients drugs designed to treat certain cancers, macular degeneration, and a range of other diseases. Researchers involved with the project say the gel is an improvement on existing drug-delivery methods, which are either quickly dispersed away from the target site or require invasive implantation.
As vehicles for medication, polymer gels link together to form a nearly unbreakable bond. A drawback, however, is that moving from pliable to durable isn’t easily accomplished. One of the goals of the research was to cut the overall work time in half.
“Now you have a gel that can change shape when you apply stress to it, and then, importantly, it can re-heal when you relax those forces,” said Mark Tibbitt, a postdoctoral researcher at MIT’s Koch Institute for Integrative Cancer Research and one of the lead authors, in a university release. “That allows you to squeeze it through a syringe or a needle and get it into the body without surgery.”
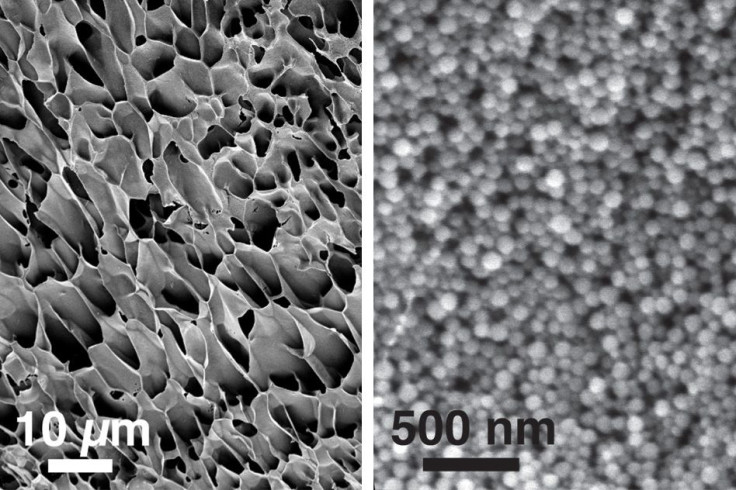
Another benefit, Tibbitt says, is the gel’s simple construction. The team created a mesh network using nanoparticles composed of PEG-PLA copolymers, which were first developed decades ago in the lab of Robert Langer, a professor at MIT and a senior author on the paper. Those particles then get entwined with a polymer made of cellulose.
“We’re working with really simple materials,” Tibbitt said. “They don’t require any advanced chemical functionalization.”
In changing the delivery method, the team is changing the drugs’ efficacy, too. Typical drug deliveries use a liquid solution, which disperse throughout the body after injection. But since the hydrogel quickly hardens near the desired tissue, drugs stay localized. This not only reduces the necessary amount of the drug a patient needs, but allows doctors to control the timing of multiple drugs that get delivered together.
Early tests mostly involve macular degeneration, an incurable and often age-related breakdown of the part of the eye responsible for acuity. Though the condition can’t be stopped, it can be slowed. Patients receive monthly injections to stem the growth of blood vessels that interfere with vision. With the new hydrogel, a timed release could cut down on the number of injections six-fold.
For cancer patients, the hydrogel would attack tumors that get left behind after surgery. If left unabated, residual cancer cells can multiply and reappear in the body with greater force. “Removing the tumor leaves behind a cavity that you could fill with our material, which would provide some therapeutic benefit over the long term in recruiting and killing those cells,” said Eric Appel, co-lead author on the paper. “We can tailor the materials to provide us with the drug-release profile that makes it the most effective at actually recruiting the cells.”
Right now, the experiments are confined to rat models. In future tests, the team eventually hopes to scale the research to human trials. With its broad application and appeal, the gel could bring sweeping relief for otherwise highly invasive, morale-draining procedures.
Source: Appel E, Tibbitt M, Webber M, Mattix B, Veiseh O, Langer R. Self-assembled hydrogels utilizing polymer–nanoparticle interactions. Nature Communications. 2015.
Published by Medicaldaily.com



























