A Simple Blood Test May Detect Breast Cancer Up to a Decade in Advance
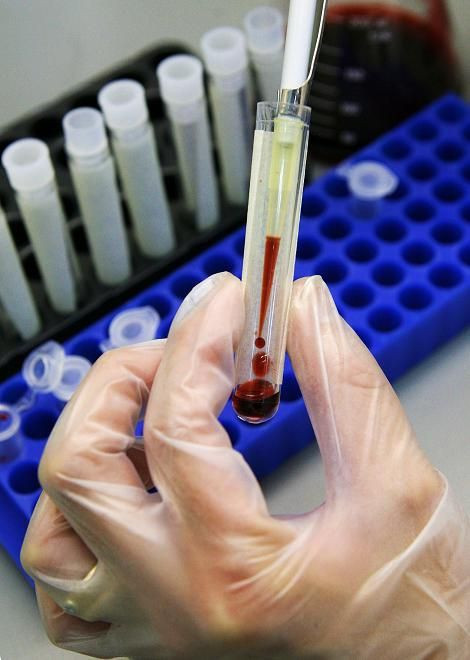
A new blood test capable of identifying a genetic change that doubles the risk of breast cancer may be able to predict the disease up to a decade before it is diagnosed, potentially allowing women to take preventative medicines and switch to healthier lifestyles before developing the tumor, according to a new study.
Researchers from the study, published in the journal Cancer Research, analyzed historic blood samples from 1,381 women of various ages, 640 of whom had developed breast cancer, and found a significant association between molecular modification of a white blood cell called ATM and the risk of developing the disease later on.
The findings show that women with the highest levels of a chemical effect called methylation, which acts like a “gene switch” on the ATM gene, were two times more likely to develop breast cancer compared to those with the lowest levels of methylation.
Blood tests were generally carried out three years before medical diagnosis, and in some incidences researchers were able to predict the discovery of breast cancer by up to 11 years, and investigators noted that the results were particularly clear for women under the age of 60.
The latest findings suggest that because molecular or ‘epigenetic’ changes in the ATM white blood cell appeared to be a DNA methylation marker for breast cancer, a simple blood test in the future could be able to determine women who are most at risk for the disease, years before tumors begin to develop.
Researchers said that DNA methylation is an "epigenetic" mechanism that allows genes to be influenced by environmental factors like hormones, radiation, alcohol, smoking and pollution.
Researchers say that epigenetic effects are increasingly being regarded as important drivers of cancer because more new research has demonstrated how chemical modifications to DNA, which controls a person’s genes, could be even more critical than DNA alone in deciding how the body’s cells grow.
“We know that genetic variation contributes to a person’s risk of disease. With this new study we can now also say that epigenetic variation, or differences in how genes are modified, also has a role,” lead author Dr. James Flanagan, of Imperial College London said in a university statement released on Tuesday.
“We hope that this research is just the beginning of our understanding about the epigenetic component of breast cancer risk and in the coming years we hope to find many more examples of genes that contribute to a person’s risk. The challenge will be how to incorporate all of this new information into the computer models that are currently used for individual risk prediction,” Flanagan said.
It is still unclear why breast cancer risk is linked to changes in a white blood cell, but previous research has also linked the ATM gene to a number of other cancers like lymphoma and leukemia.
“So far we have found alterations in one small region of a gene that appear to associate with risk of disease and so the next step with this epigenetic research is a genome wide approach to try and find all the associated genes,” Flanagan said.
Flanagan said that combined with other information like family history, a blood test to determine the methylation levels of the white blood cell gene would help spot women who could benefit from preventative cancer measures.
“Dr. Flanagan’s research into epigenetics is so exciting because it suggests that there is every possibility that the risk of developing breast cancer could be decided many decades in advance. By piecing together how this happens, we can look at ways of preventing the disease and detecting it earlier to give people the best possible chance of survival,” Baroness Delyth Morgan, Chief Executive of Breast Cancer Campaign said in a statement.
Published by Medicaldaily.com



























