Simply Using Antibiotic Soap And Ointment Lowers MRSA Superbug Infections In ICU By 37%
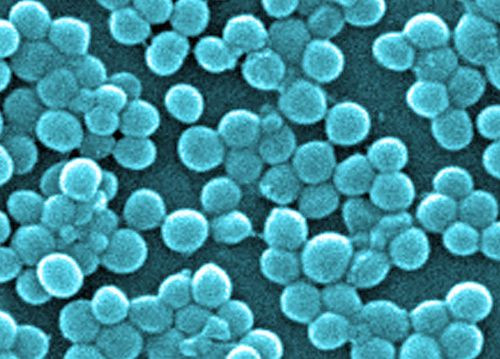
Methicillin resistant Staphylococcus aureus (MRSA) is the scourge of current hospital-related infections. In 2005, 18,000 people in the U.S. died from the bacterial infection, a number that topped deaths from AIDS, according to the Centers for Disease Control and Prevention (CDC). The infection is often picked up in hospital settings where improper cleaning or handling of patients can spread the infection. It is for this reason that pharmaceutical companies are racing toward developing new antibiotics to battle the infection, the name of which suggests that it is resistant to the last line of defense antibiotic methicillin. But a newly published report in the New England Journal of Medicine shows that a simple change in procedure could stop a large percentage of infections in hospital settings.
The CDC performed the study, which tried two small changes to the care of intensive care unit (ICU) patients, in order to determine what simple steps could be taken to limit the spread of the deadly bacteria. The results, looking at more than 74,000 patients across 74 ICUs in the U.S., showed that general infections could be reduced by 44 percent in the most vulnerable patients and MRSA infections could be reduced by 37 percent. This is welcome news as 75 percent of all Staph infections in hospitals are drug-resistant.
The patients used in the experiment were split into three groups. In the first group, ICU patients were screened for MRSA and were isolated if they were found to be carriers. The second group followed the same protocol but patients who were carriers were washed with chlorohexadine (a type of antibiotic) soap and used common antibiotic ointment, mupirocin, on the insides of their noses for five days. The third group was not screened and were all treated with the antibiotic soaps and ointment.
Interestingly, the rates of ICU patients being carriers for MRSA strains dropped by a staggering 37 percent in the group where all patients were treated, but not significantly in either of the other two groups. The study showed that simple procedures could stop the spread of MRSA as well as other infectious bacteria, leading to healthier patients.
"This study helps answer a long-standing debate in the medical field about whether we should tailor our efforts to prevent infection to specific pathogens, such as MRSA, or whether we should identify a high-risk patient group and give them all special treatment to prevent infection," said lead author Susan Huang, M.D., M.P.H., associate professor at the UCI School of Medicine. "The universal decolonization strategy was the most effective and the easiest to implement. It eliminates the need for screening ICU patients for MRSA."
Researchers from University of California, Irvine, Harvard Pilgrim Health Care Institute, Hospital Corporation of America, and the CDC all ran the study together. "CDC invested in these advances in order to protect patients from deadly drug-resistant infections," said CDC Director Dr. Tom Frieden, M.D., M.P.H. "We need to turn science into practical action for clinicians and hospitals. CDC is working to determine how the findings should inform CDC infection prevention recommendations."
Source: Huang S, Septimus E, Kleinman K, et al. Targeted versus Universal Decolonization to Prevent ICU Infection. New England Journal of Medicine. 2013.



























