Single Endoscopic Treatment Could Eliminate Need For Insulin In Type 2 Diabetes Patients
A new "disease-modifying" single endoscopic treatment could eliminate the need for insulin therapy in type 2 diabetes patients, a recent study has revealed.
An hour-long procedure of sending electronic pulses to the small intestine could allow patients with type 2 diabetes to stop taking insulin and still maintain glycemic control, researchers have said.
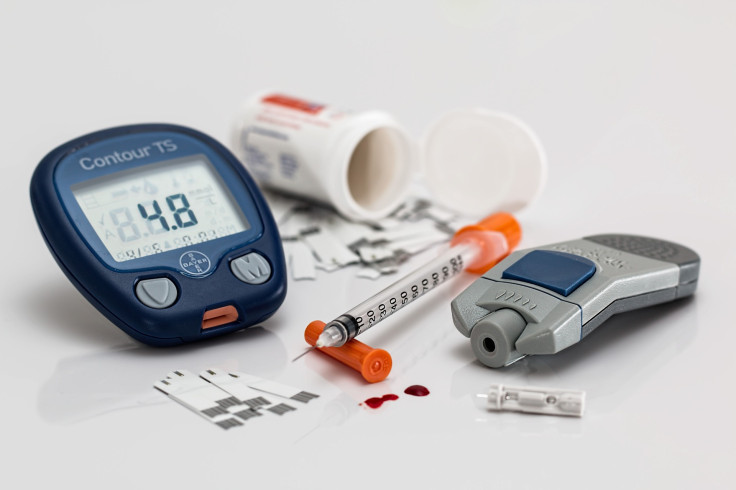
Insulin is a hormone released by the pancreas that signals body cells to open up to convert glucose into energy. However, people with type 2 diabetes face insulin resistance, a condition in which cells in the muscles, fat and liver do not respond to insulin, resulting in excessive sugar in the blood. Hence, insulin therapy is vital for those people to prevent diabetes complications by keeping their blood sugar within the target range.
The new study will be presented at Digestive Disease Week, an annual meeting of gastrointestinal experts, next week. The treatment may give a ray of hope for around 150–200 million people worldwide who depend on insulin therapy for maintaining blood sugar levels.
It is estimated that more than 30 million people live with diabetes in the U.S., out of which around 7.4 million depend on insulin to manage their condition.
"The potential for controlling diabetes with a single endoscopic treatment is spectacular," Celine Busch, the study's lead researcher from Amsterdam University Medical Center, said in a news release. "One of the biggest advantages of this treatment is that a single outpatient endoscopic procedure provides glycemic control, a potential improvement over drug treatment, which depends on patients taking their medication day in, day out."
Researchers earlier found that patients who underwent gastric bypass had improved insulin control immediately after the surgery, even before they had experienced any weight loss. This led researchers to conclude that the duodenum, the portion of the lining of the small intestine just below the stomach, plays a key role in glycemic control in type 2 diabetes. This prompted researchers to use ablation procedures to modify the cells in the area.
Although the exact cause of insulin resistance is still not known, researchers believe chronic exposure to a high-sugar, high-calorie diet can cause changes to the small intestine that can result in insulin resistance.
Researchers hypothesized that rejuvenating the portion of the small intestine would improve the body's ability to respond to insulin.
As part of the study, 14 patients underwent the endoscopic treatment which involves sending alternating electrical pulses to the duodenum. The patients were discharged on the same day and were placed on a calorie-controlled liquid diet for two weeks. They were asked to take semaglutide, a diabetes medicine, of up to 1 mg a week.
Semaglutide was found to have improved insulin glycemic control in type 2 diabetes patients in about 20% of cases. The latest study showed that 12 of 14 patients, (86%) maintained good glycemic control without insulin for a year, indicating the success was from endoscopic procedure and not just to the use of semaglutide.
"While drug therapy is 'disease-controlling,' it only reduces high blood sugar as long as the patient continues taking the medication," said Jacques Bergman, an investigator on the study and professor of gastrointestinal endoscopy at Amsterdam University Medical Center.
"This one procedure is 'disease-modifying' in that it reverses the body's resistance to its own insulin, the root cause of type-2 diabetes," Bergman added.
Published by Medicaldaily.com



























