Slade Dill, Idaho Boy, Survives Flesh-Eating Bacteria That Began As Cut On His Leg
Slade Dill, an eighth-grader from Twin Falls, Idaho, returned home on Monday after surviving a run-in with deadly flesh-eating bacteria. Doctors at Primary Children’s Hospital in Salt Lake City even held off on amputating the boy’s leg because they didn’t think he would survive long enough.
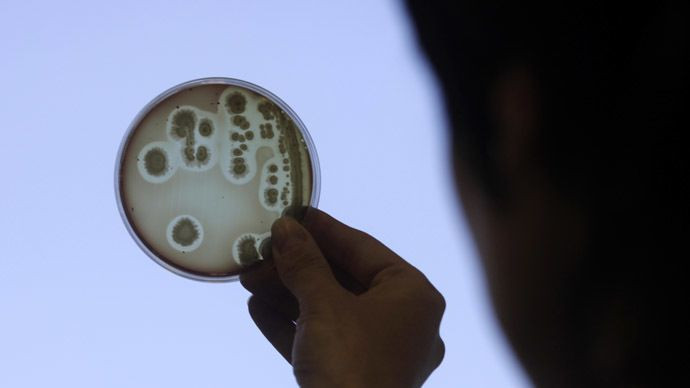
"The disease is easy to misdiagnose. It may start with a red spot on the skin," Twin Falls dermatologist, Chris Scholes, told Twin Falls Times-News. "The infection goes deeper beneath the skin and can move relatively quickly and get serious fast."
Slade’s nightmarish journey started on Sept. 20 when a scrape on his knee started to swell. By Sept. 22, he started to experience pain in multiple areas of his body. After doctors at St. Luke’s Magic Valley located fluid in his abdomen and chest through a CT scan, he was flown to Primary Children’s Hospital, where he was rushed into emergency surgery. He was soon after diagnosed with necrotizing fasciitis.
According to the Centers for Disease Control and Prevention, necrotizing fasciitis, also known as flesh-eating bacteria, is a severe bacterial infection that destroys the body’s soft tissue. People who take care of open wounds, practice proper hygienic care, and have healthy immune systems tend to avoid contracting this rare disease.
Following surgery to remove dead tissue, Slade returned home on Monday and has been given a strict regimen of antibiotics. “Whatever they say, we are going to do it and be thankful,” Slade’s mother, Dixie Dill, told Twin Falls Times-News.
To help the Dill family pay for Slade’s medical bills, the local Wells Fargo Bank branch has set up a fundraising account in his name.
Earlier this week, 79-year-old George Clark became the 27th person infected with another flesh-eating bacterium known as Vibrio vulnificus. Clark was treated at Baptist Medical Center in Jacksonville after he was pinched by a crab that was most likely carrying the disease.
Vibrio vulnificus is part of the same bacteria family that causes cholera and is normally found in warm seawater. Patients usually develop an infection through contaminated seafood or seawater exposure to an open wound.



























