T-Cells Have Pain Receptors On Their Surfaces; Manipulating Them Could Treat Autoimmune Disorders
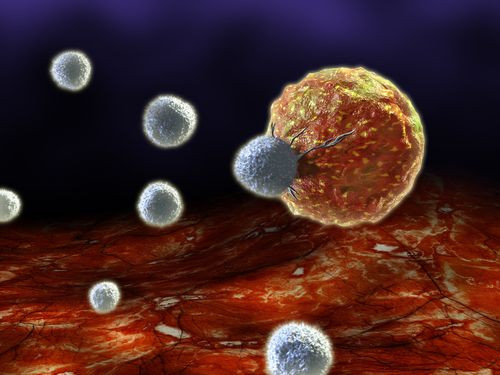
T-cells, with their ability to seek and flush out microbial pathogens, are among the most important components of our immune system. But T-cells can function only when they're able to remember the pathogens they're fighting, at which point they become effector T-cells. New research into the function of T-cells finds that this transformation is triggered by a pain receptor on the surface of T-cells.
The study, published in Nature Immunology, also shows that the pain receptor can be manipulated to make T-cells more responsive to medical interventions for autoimmune diseases, such as Crohn’s and multiple sclerosis. Blocking it entirely even cured intestinal inflammation in mice.
T- cells are activated when they encounter antigen-presenting cells, or cells with a substance on them that evokes an immune response. Although other receptors have previously been found to activate T-cells, the current research finds a new receptor, from the TRPV1 channel. The receptor already plays a role in activating nerve cells that help regulate body temperature, and alert the brain to heat and pain. It's also been called the capsaicin receptor because it produces the burning sensation people experience when they touch chili peppers. When TRPV1 activates on the T-cells, there's an increase in intracellular calcium ion levels — a process needed for T-cells to activate.
"Our study breaks current dogma in which certain ion channels called CRAC are the only players involved in calcium entry required for T-cell function," lead author Samuel Bertin said in a statement. "Understanding the physical structures that enable calcium influx is critical to understanding the body's immune response."
This T-cell activation is essential to fighting infections. People with AIDS have compromised immune systems in which T-cells are fighting for their lives against the virus — the destruction of these cells renders the body defenseless afainst normally harmless pathogens. Conversely, an abundance of T-cells can help people naturally acquire immunity to some diseases, and certain vaccines have been developed to exploit this process. Autoimmune disorders, meanwhile, occur when T-cells mistake harmless substances within the body — or even organs and tissue — as pathogenic. Allergies are one example of these types of conditions. Crohn's disease is another one, in which the immune system turns against the gastrointestinal tract. In all, autoimmune disorders affect more than 23.5 million Americans.
The new research applies to these conditions because the scientists found that T-cell responses can be manipulated through the TRPV1 channel. Specifically, researchers found in in vitro experiments that the T-cell inflammatory response could be reduced by blocking the gene that encodes for the protein comprising the TRPV1 channel. Overexpression of this gene is what leads to excess T-cell activationm which in turn causes autoimmune diseases. T-cells also responded to pharmaceutical agents that block or activate the TRPV1 channel.
The researchers showed how TRPV1 was blocked in mice with colitis using an already developed painkiller. The drug was administered at even lower doses than would normally be used to treat pain. "This suggests we could potentially treat some autoimmune diseases with doses that would not affect people's protective pain response," senior author Eyal Raz said in the statement.
Source: Lee J, To K, Raz E, et al. Nature Immunology. 2014.



























