There’s A Blood Test To Predict Just About Everything, But How Much Would You Want To Know?
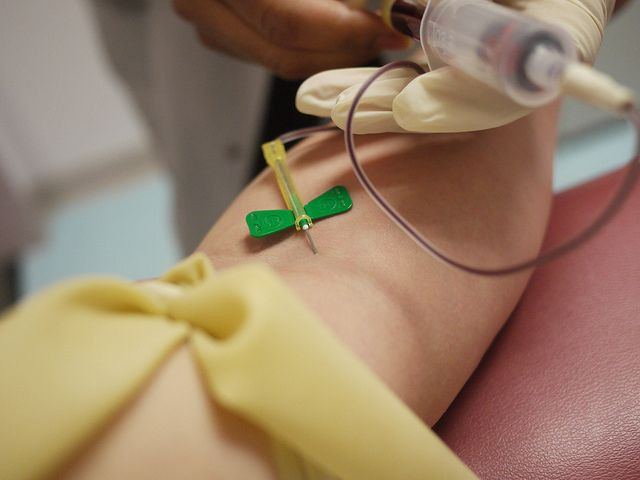
Your bloodstream is a messy, tumbling universe of many inhabitants — all of them racing around, eternally hurried, never quite finishing the work they intended to do. Luckily, medical science has made something of an art of capturing this chaos, as the common blood test is perhaps the most useful tool we have to assess a person’s health.
We’re getting so good, in fact, that just about every major disease has been found, in some capacity, to show up as certain risk factors in a blood test. These include: concussions, cancers, obesity, heart attack, cataracts, developmental delays in newborns, multiple sclerosis, Alzheimer’s disease, fibromyalgia, diabetes, and even death. Countless lives have been saved as a result of these diagnoses, yet on an individual level an important question persists: How much speculation about your health is too much?
For blood tests to mean anything, scientists need to find telltale “biomarkers.” Basically, biomarkers are the red flags in your blood. They can be substances or states, meaning they can be specific tracers introduced into the body, like in the case of certain radioactive isotopes that rainbow under an X-ray, or they can be electrical signals coming from your brain.
Biomarkers also exist naturally in your body. Such is the case with prostate-specific antigens, or PSA. Over time, science has discovered that the greater presence of PSA has a direct correlation to the size of a man’s prostate, which could indicate the incidence of cancer. Blood tests rely on these naturally-occurring associations: The higher your number is, the greater your chance is for some known disease or condition.
The problem is, biomarkers aren’t perfect. PSA tests, for instance, have a notoriously high false-positive rate. They’re highly sensitive in their testing but equally unspecific. In other words, while they are quite good at detecting cancer, they tend to overestimate what else is going on, which means doctors may order painful follow-up biopsies even though there is no cancer present.
Doctors, for their part, may be falling into something of a statistical trap. One 1982 study asked physicians a hypothetical question. The skeleton of the problem has been changed multiple times over the decades, but the effect is equally perplexing: John says he’s itchy. There’s an allergy test that can determine whether he has allergies, but like other tests, it comes with a false-positive risk. In this case, it’s 10 percent. The question is: If one percent of the population has the allergy and John’s test results say “Yes,” what are the chances he actually has the allergy?
The correct answer, to many people’s surprise, is seven percent. “Unfortunately,” the researchers wrote, “most physicians (approximately 95 out of 100…) misinterpret the statements about the accuracy of the test and estimate [the prevalence rate] to be about 75%.” Their thinking was backward, the researchers point out. They assumed that the chances John had an allergy given a positive test result were equal to the chances of a positive test result in a patient with cancer. The difference is subtle, but hugely important. “The latter probability is the one measured in clinical research programs and is very familiar, but it is the former probability that is needed for clinical decision making.”
Now multiply these simple errors in reasoning across the dozens of blood tests currently available to patients. Blood tests may be reliable indicators of fat levels and cholesterol in the blood, but when it comes to associating the results with larger, more urgent diseases — especially those that come with painful or costly treatment regimens — not all information can be trusted. Now more than ever, patients should stick to the sage advice: Get a second opinion.
Published by Medicaldaily.com



























