Treating Brain Tumor with Old Drugs
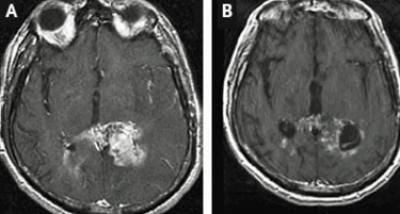
Scientist found that two drugs, already being used to treat other forms of cancer has prolonged the survival of mice modeling a particular form of the most common type of malignant brain tumor, glioblastoma.
Researchers at the University of California, San Diego School of Medicine and UC San Diego Moores Cancer Center, in collaboration with colleagues in Boston and South Korea, also identified a “novel gene mutation” that causes at least one form of glioblastoma (GBM).
As more than 9,000 new cases of the disease in the U.S. are diagnosed each year and effective treatments are limited, these findings could be “good news for at least some GBM patients,” the authors write.
While the tumors are aggressive and resistant to current therapies, such as surgery, radiation and chemotherapy, the researchers explained that the median survival rate for newly diagnosed GBM patients is just 14 months.
Past studies have identified epidermal growth factor receptor (EGFR) as a common genetically altered gene in GBM, though the cause or causes of the alteration is not known, the authors wrote.
“The research team, led by scientists at the Dana-Farber Cancer Institute in Boston, analyzed the GBM genomic database, ultimately identifying and characterizing an exon 27 deletion mutation within the EGFR carboxyl-terminus domain (CTD).”
They explained that an exon is a segment of a DNA or RNA molecule containing information coding for a protein or peptide sequence.
"The deletion mutant seems to possess a novel mechanism for inducing cellular transformation," said Frank Furnari, PhD, associate professor of medicine at the UC San Diego School of Medicine and an associate investigator at the San Diego branch of the Ludwig Institute for Cancer Research.
The researchers explained that they determined that “cellular transformation was induced by the previously unknown EGFR CTD deletion mutant, both in vitro and in vivo, and resulted in GBM in the animals, researchers then turned to testing a pair of approved drugs that target EGFR: a monoclonal antibody called cetuximab and a small molecule inhibitor called erlotinib.”
Cetuximab, marketed under the name Erbitux, is currently approved for use in treating metastatic colorectal cancer and squamous cell carcinoma of the head and neck. Erlotinib, marketed under the name Tarceva, is used to treat lung and pancreatic cancers.
Researchers found that both drugs effectively impaired the tumor-forming abilities of oncogenic EGFR CTD deletion mutants.
They said that Cetuximab prolonged the survival rate of mice with the deletion mutants when compared to untreated control mice.
However, while the drugs work by binding to sites on the EGFR protein and inhibiting activation, they are not effective in all cancer patients and produce some adverse side effects, such as rashes and diarrhea.
But Director of Neuro-Oncology at UC San Diego Moores Cancer Center and the UCSD Department of Neurosciences and co-author Santosh Kesari, MD, PhD, said the new study proves a more effective use of the drugs for some patients with GBM.
"In the past when we treated brain cancer patients with these drugs, the response rate was very small," Kesari said.
"What we now show is that the tumors with CTD mutations respond best to these EGFR targeted agents. If we knew this beforehand, we might have been able to select patients most likely to respond to these agents. We are now trying to put together a prospective clinical trial to prove this. We would select only patients with these tumor mutations and treat them. This kind of research gets us closer to identifying genetic subtypes, to doing better biomarker-based clinical trials, and to personalizing treatments in brain cancers."
"This is a great example of personalized medicine in action," said Webster Cavenee, PhD, director of the Ludwig Institute at UC San Diego.
"UCSD has made a concerted effort in the past few years to develop a first-class brain tumor research and therapy group that includes adult neuro-oncology, neurosurgery, neuropathology and their pediatric equivalents to join with internationally-renowned brain tumor research. This is making UCSD a destination for the very best in brain tumor management."
Published by Medicaldaily.com



























