Stem Cells Of Type 1 Diabetes Patients Transformed Into Insulin-Secreting Beta Cells; Research May Lead To New Therapy
For those living with Type 1 diabetes, the condition is a part of daily life. Insulin shots, blood sugar monitoring, and carb counting become routine, and patients expect them to stay so for the rest of their lives. This form of diabetes currently has no cure, something researchers have been diligently trying to change. The most recent attempt to take down diabetes comes from researchers at Washington University School of Medicine in St. Louis and Harvard University, who have managed to change stem cells derived from diabetes patients into insulin–secreting cells.
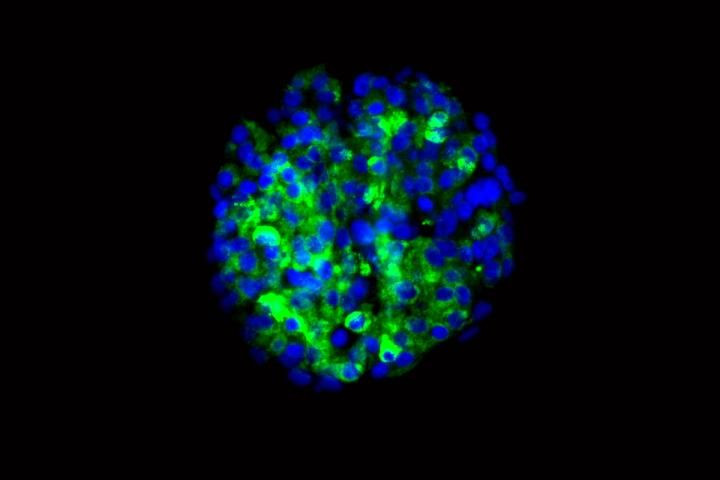
Patients with Type 1 diabetes lack the ability to create their own insulin, meaning they rely on regular injections of the hormone to control blood sugar. The study hints at a possible new therapy for patients that relies on a personalized approach — using the patients’ own cells to create new ones capable of manufacturing the insulin they need. The research, published in Nature Communications, details new cells that produce insulin when they encounter sugar in both culture and mouse trials.
“In theory, if we could replace the damaged cells in these individuals with new pancreatic beta cells — whose primary function is to store and release insulin to control blood glucose — patients with type 1 diabetes wouldn’t need insulin shots anymore,” said Dr. Jeffery R. Millman, an assistant professor of medicine and biomedical engineering at Washington university and first author of the study, in a press release. “The cells we manufactured sense the presence of glucose and secrete insulin in response. And beta cells do a much better job controlling blood sugar than diabetic patients can.”
Millman had conducted previous studies involving the creation of beta cells derived from people who did not suffer from diabetes. In the new experiment, however, the stem cells used come from the skin of Type 1 diabetes patients.
“There had been questions about whether we could make these cells from people with type 1 diabetes,” MIllman said. “Some scientists thought that because the tissue would be coming from diabetes patients, there might be defects to prevent us from helping stem cells differentiate into beta cells. It turns out that’s not the case.”
The idea of replacing beta cells is actually more than two decades old, originating with Washington university researchers Dr. Paul E. Lacy and David W. Sharp, who began transplanting such cells into Type 1 diabetes patients. Today, there has been some success with beta cell transplants, but these cells come from pancreas tissue provided by organ donors. As with all donated types of tissues, cells, and organs, the supply falls short of the demand. The new technique would solve this problem, but Millman said scientists need to conduct more research to make sure the new cells don’t cause tumor development — a problem that has cropped up in many types of stem cell research. There has been no evidence of tumors so far in the mice, though, even up to a year after cell implantation.
Millman predicts the stem cell-derived beta cells could be ready for testing in humans in three to five years. This process would consist of implanting the cells under the skin of diabetes patients, a minimally invasive procedure that would give the cells access to a the patient’s blood supply.
“What we’re envisioning is an outpatient procedure in which some sort of device filled with the cells would be placed just beneath the skin,” he said.
Millman said that the technique could, in the future, even be used to help those with Type 2 diabetes, neonatal diabetes, and Wolfram syndrome.
Source: Millman J, Xie C, Van Dervort A, Gurtler M, Pagliuca F, Melton D. Generation of Stem Cell-derived B-cells from Patients with Type 1 Diabetes. Nature Communications. May 10, 2016.



























